FAQs about myasthenia gravis
The life expectancy for people with myasthenia gravis generally falls in line with normal ranges, and many patients are able to live full, active lives. Some patients also may achieve disease remission for long periods of time, or permanently.
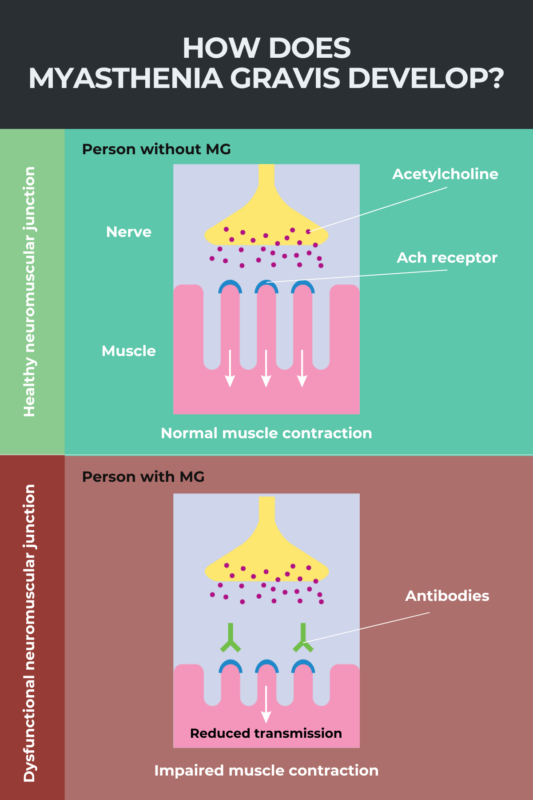
Myasthenia gravis has an autoimmune origin and is not typically considered a heritable disease. Some people may have mutations in genes that affect the function of proteins involved in nerve-muscle communication and cause congenital myasthenia, but this is considered to be a distinct clinical condition.
Myasthenia gravis is estimated to impact about 14-40 people per 100,000 in the U.S., and about 150-200 people per million worldwide. Because it affects fewer than 200,000 people in the U.S., the condition is considered a rare disease.
Myasthenia gravis may be diagnosed with a range of different tests. A blood test looking for the presence of disease-causing antibodies is the main way of diagnosing myasthenia gravis. In some cases, additional nerve-muscle function tests or other evaluations may be necessary to reach a definitive diagnosis of myasthenia gravis.
There is no cure for myasthenia gravis (MG), but a number of medications and other treatments are available that can help ease its symptoms and boost patients’ quality of life. Some patients may achieve temporary or permanent disease remission with or without the help of treatments.
Related Articles

 Fact-checked by
Fact-checked by