Myasthenia gravis ice pack test
Last updated Nov. 8, 2024, by Agata Boxe

The ice pack test is a simple diagnostic tool that may help identify myasthenia gravis (MG) in just a few minutes, especially if your MG symptoms include droopy eyelids.
The test involves placing an ice pack on the affected eyelid. The cold temperature tends to reduce the droop by improving muscle strength. It does not usually have an effect on people who do not have the disease, which is why it is useful to help make an MG diagnosis.
The ice pack test for MG is typically done by an ophthalmologist or a neuro-ophthalmologist, but it is not considered a definitive MG test. If the eyelid droop responds to the test, other assessments will be needed to confirm the MG diagnosis.
What is the ice pack test for myasthenia gravis?
MG is a neuromuscular condition in which the immune system mistakenly targets proteins needed for nerve and muscle cells to communicate, causing the hallmark symptoms of muscle weakness and fatigue.
Ptosis, or a drooping in the upper eyelids, is a common symptom of ocular MG, a type of MG that affects only the eyes. However, eyelid drooping is also frequently observed in generalized MG, the most common form of MG with symptoms that include widespread muscle weakness, and fatigue.
The ice pack test for MG works by cooling the eyelid muscles, which makes them contract and causes the drooping to improve noticeably after the ice pack is removed. If the droop is reduced by more than 2 mm, the test is considered positive.
The test was developed after observations that muscle weakness caused by MG often worsens with heat and improves when exposed to cold. Still, the test’s mechanism for improving symptoms is not fully understood.
Scientists believe several mechanisms might lead to a stronger contraction of eyelid muscles after exposure to cold temperatures. For example, cold may lead to a greater accumulation of signals from nerve cells that tell muscles to contract. The transmission of chemical signals also seems to be more efficient at cold temperatures, and muscle cells have a generally stronger contractile response after cooling.
Over the years, the use of the ice pack test in MG diagnostics has increased because it is inexpensive, noninvasive, and accurate. In a 2023 review study, collected data from 20 studies that used the test in patients with ocular MG symptoms showed 73%-100% of patients were correctly identified with the test.
The sensitivity demonstrated in the study was not better than that of single-fiber electromyography (EMG), which is considered the most sensitive test for MG, but the ice pack test may still prove useful to doctors who don’t have access to EMG.
An alternative to the ice pack test for diagnosing MG had been the Tensilon test, but it was discontinued in the U.S. in 2018 because of high rates of false positive results and rare side effects.
How to perform the ice pack test
The MG ice pack test should be done by an ophthalmologist or a neuro-ophthalmologist. They can tell you what the results mean and guide you about next steps, including whether you should undergo other tests or receive MG treatment.
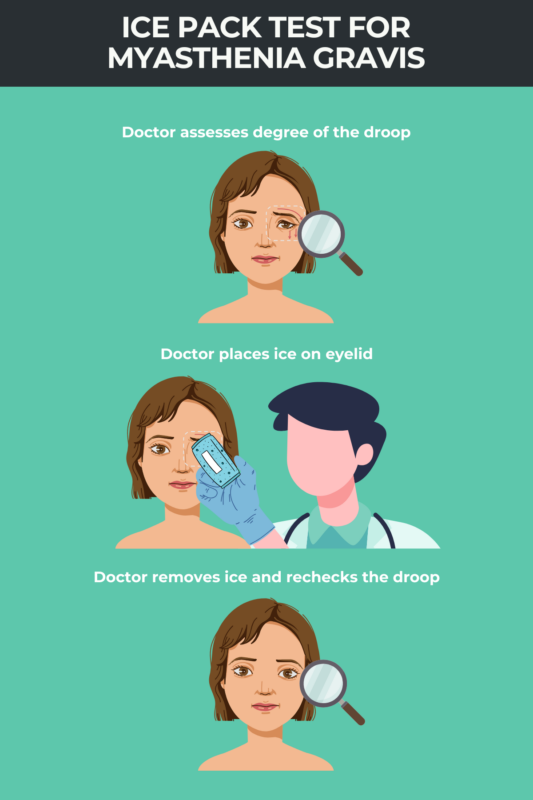
The MG ice pack test involves the following steps:
- Preparation: The doctor will prepare the ice pack, which is usually crushed ice wrapped in a clean plastic bag and a cloth, or they may fill a surgical glove with ice. Before applying the ice pack, they will document the degree of the eyelid droop by taking photos and measuring the extent of the droop with a ruler.
- Application: The doctor will ask you to sit down. They will then place the ice pack on one or both eyelids for about two to five minutes. When the ice pack is removed, you will be asked to look straight ahead.
- Observation: The doctor will take more photographs and eyelid droop measurements, which will be compared to the ones taken earlier.
You may want to learn how to do the ice pack test for MG at home, as it seems straightforward. However, Amanda Henderson, MD, chief of the neuro-ophthalmology division at the Johns Hopkins Wilmer Eye Institute in Baltimore, Maryland, recommends that a doctor does it for the most accurate interpretation of results.
“I think, in general, self-diagnosis is not really advised,” she says. “So I think it’s reasonable for it to be performed by a doctor, although it’s not going to harm anyone.”
The doctor will know how to do the MG test correctly by checking that the pack is applied evenly and that the temperature of the room doesn’t affect the results.
For potential ocular MG symptoms, your doctor may also conduct fatigability testing, where you are asked to look up for about two to three minutes. When a person has ocular MG symptoms, the eyelid muscles become tired from gazing upward and continue to droop, indicating a potential MG diagnosis.
Is the ice pack test safe?
The ice pack test for MG is considered safe because it is noninvasive and does not involve medication. Possible minor risks include skin irritation and discomfort from cold exposure, especially for people with sensitive skin.
A doctor will make sure the ice does not stay on the eyelids for too long, which can decrease the eyelid muscles’ ability to contract, potentially affecting the accuracy of results and leading to a false negative test.
Another precaution to prevent ice burns is to cover the ice pack with material that protects the skin from having direct contact with the ice.
Results and next steps
Only a doctor can correctly interpret the results of an MG ice pack test, which is just one of many tests considered when making an MG diagnosis.
“I don’t treat it as a definitive test,” says Henderson.
A positive ice pack test for MG means the eyelid that was previously droopy lifts up, which supports an MG diagnosis, explains Henderson. If the eyelid position doesn’t change, it is a negative result, which does not suggest a diagnosis of the disease, she says.
However, a positive result also typically signals a need for further testing to confirm a diagnosis, and a negative test does not rule out MG entirely.
“I think there are really not many of us who are treating purely based on the results of this test,” Henderson says. “The diagnosis of myasthenia involves a lot of different data.”
Some of the additional tests your doctor may recommend include EMG, blood tests, and imaging studies.
Myasthenia Gravis News is strictly a news and information website about the disease. It does not provide medical advice, diagnosis, or treatment. This content is not intended to be a substitute for professional medical advice, diagnosis or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website.
Recent Posts
- Working through myasthenia gravis, one story at a time
- Azathioprine eases MG symptoms, but does not extend survival: Study
- How studying history can help us navigate life with chronic illness
- Povetacicept reduces disease activity in MG mouse model
- The tug-of-war between my independence and his caregiving
Related articles