FAQs about types of myasthenia gravis
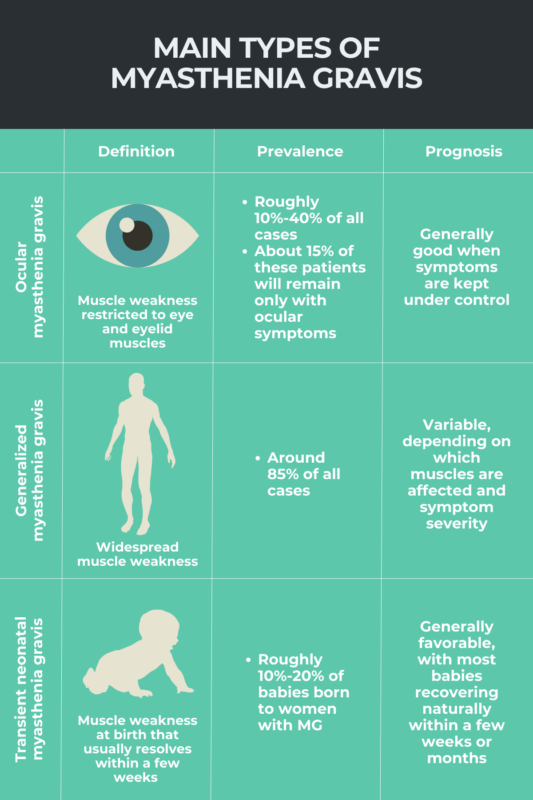
Many patients who start having symptoms of ocular myasthenia gravis will later progress to generalized myasthenia gravis; thus, the generalized form of the condition is the most common type of the disease. By subtype, patients who are positive for antibodies targeting the acetylcholine receptor protein, known as AChR, account for the large majority of cases, about 85% in all.
Myasthenia gravis can present with a range of clinical severities, regardless of disease type. Nevertheless, generalized myasthenia gravis may be considered the most severe form of the condition because it can affect respiratory muscles, potentially leading to life-threatening complications known as myasthenic crises.
Patients with any type of myasthenia gravis may have more or less severe disease. For adults, ocular myasthenia gravis is typically less severe than generalized myasthenia gravis because muscle weakness is restricted to muscles controlling eye and eyelid movements.
According to the National Organization for Rare Disorders (NORD), there are three main types of myasthenia gravis: ocular, affecting just the eyes; generalized, which can impact many muscles in the body; and transient neonatal, occurring among some babies born to women with MG. Patients also can be further divided into subtypes of the disease based on various factors, including age at disease onset, the type of disease-causing antibodies, or the presence of abnormalities in the thymus gland.
All forms of myasthenia gravis are marked by muscle weakness and fatigue, but ocular myasthenia gravis is distinguished by the fact that weakness is limited to the muscles of the eyes and eyelids, whereas generalized myasthenia gravis may affect a wide range of muscles in the body. Transient neonatal myasthenia gravis is distinct in that it occurs specifically in babies born to mothers with myasthenia gravis and usually is temporary. A person’s doctor will be able to conduct additional tests to help each patient understand the specific diagnosis.

 Fact-checked by
Fact-checked by