FAQs about myasthenia gravis diagnosis
A number of different healthcare professionals may be involved in the diagnosis of myasthenia gravis, depending on a patient’s symptoms, and may include primary care physicians and neurologists. In many cases, eye-related problems are among the first symptoms of the disease, so ophthalmologists may play a role in the diagnosis of myasthenia gravis.
As with many diseases, an earlier diagnosis of myasthenia gravis typically is associated with a sooner start on treatment and more beneficial outcomes. If myasthenia gravis is left untreated, muscle weakness may progress faster and patients may be at a higher risk of experiencing myasthenic crises, a life-threatening disease complication. Still, every person’s disease course differs and there is no way of knowing exactly how a person’s disease will progress either with or without a diagnosis.
The length of time it will take to receive the results of a blood test for myasthenia gravis depends on several factors and will vary by testing location. In general, it may range from a few days to a few weeks. Patients who undergo blood testing for the disease should speak with their healthcare team about when they can expect results.
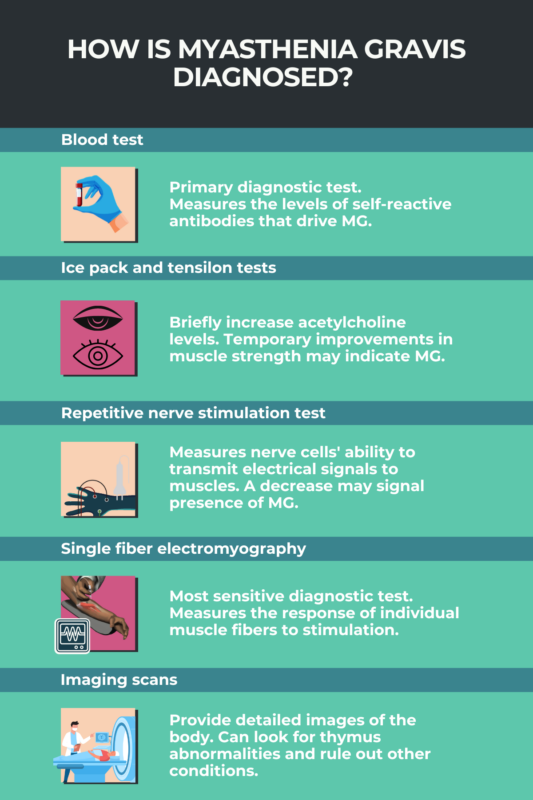
After a thorough physical and neurological exam, a blood test looking for common myasthenia gravis-causing antibodies is the main way doctors diagnose the disease. In some cases, physicians may use a range of other tests to assess a person’s nerve and muscle function to confirm the diagnosis.
Whether a test for myasthenia gravis will be covered by health insurance will depend on a person’s individual healthcare plan. Patients should speak with their insurance provider to understand the type of coverage they have. The National Organization for Rare Disorders (NORD) has a patient assistance program for people with myasthenia gravis living in the U.S.; its goal is to offer financial support to people facing limited resources to pay for specific healthcare costs, including physician-prescribed laboratory and diagnostic tests.

 Fact-checked by
Fact-checked by