Risks for post-operative MG crisis identified in non-thymoma patients
Risks include severe disease, history of crises, and poor overall health
Post-operative myasthenic crisis is a dangerous complication after thymus removal surgery for people with myasthenia gravis (MG) who had no tumor in their thymus, according to researchers who set out to identify factors that increase this risk in a recent study.
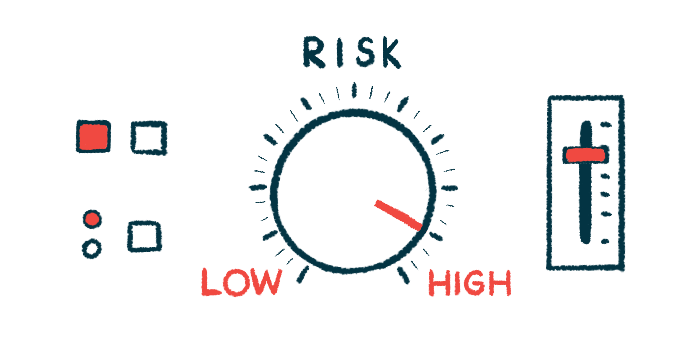
They determined risk factors to be: having a poor Osserman classification indicative of higher disease severity, a history of myasthenic crises, a higher dosage of pyridostigmine before surgery, and higher American Society of Anesthesiology (ASA) scores signaling a poorer overall health status.
Such patients “should be highly alert to the occurrence of postoperative myasthenic crisis,” researchers wrote.
The study, “Analysis of influencing factors of perioperative myasthenic crisis in 387 myasthenia gravis patients without thymoma in a single center,” was published in the Journal of Cardiothoracic Surgery.
Myasthenic crisis is most severe complication of thymectomy for MG patients
MG is a neuromuscular disease that occurs when the body’s immune system attacks proteins important for nerve-muscle communication, leading to symptoms of muscle weakness and fatigue.
Abnormalities in the thymus gland — an organ that is part of the immune system — are commonly seen in MG patients. Up to 70% of patients have an enlarged thymus, while 10%-15% have thymomas, which are tumors in the thymus that are usually benign.
Thymectomy is a surgery to remove the thymus gland and is considered a long-term treatment to allow patients to reduce or stop taking MG-related medications. A sizable proportion of patients (about 70%) experience a significant reduction in medication or achieve stable remission within a year after surgery.
The most dangerous complication of thymectomy is a myasthenic crisis — a serious complication of MG marked by severe muscle weakness and respiratory failure that requires assisted ventilation. When a myasthenic crisis occurs after surgery, it is called post-operative myasthenic crisis (POMC).
Here, researchers conducted a study with the goal of identifying risk factors for POMC in MG patients without a thymoma. The same researchers previously published a study investigating POMC risk for patients who had a thymus tumor.
The new study included a total of 387 patients — 204 men and 183 women, with a mean age of 45.9 years — who underwent a thymectomy in a Beijing hospital in China, from February 2011 to December 2021.
For the purposes of this study, a POMC was defined as an event occurring within a month after surgery. Patients experiencing POMC would require intubation or non-invasive ventilation for more than 24 hours, or would need to be re-intubated due to breathing weakness or inability to cough.
The study found POMC occurred in 45 patients (11.6%).
A univariate statistical analysis, which evaluated each variable independently, identified age, previous myasthenic crises, a daily pyridostigmine dose of 240 mg or higher, poor lung function, and blood loss over one liter during surgery as risk factors for the development of POMC.
An Osserman classification of IIb and above, indicating moderate to severe generalized MG, and an ASA grade of 2 and 3 — signaling the presence of a mild to severe systemic disease — were also associated with an increased risk of POMC.
A multivariate statistical analysis, which takes into account all factors together, confirmed that a history of myasthenic crisis and a daily dose of pyridostigmine of 240 mg or higher before surgery were independent risk factors for the development of POMC. An Osserman classification of IIb or higher, and an ASA grade of 2 and 3 were also identified as independent risk factors in this analysis.
POMC risk increases with weakness in muscles involved in eating and breathing
Patients classified as Osserman type IIb or above have weakness in muscles involved in swallowing, chewing, and breathing. Intubation during surgery may also account for these symptoms, leading to increased airway secretion and inability to cough up, which in turn may increase the risk of POMC.
“Weakness in these muscles interferes with upper airway protection, swallowing, and secretion clearance, even lead to upper airway obstruction and respiratory failure,” the researchers wrote.
A higher dosage of pyridostigmine might also decrease the ability of patients to cough up and increase the risk of respiratory infections due to the accumulation of secretions. It is also typically associated with more severe disease symptoms.
“Therefore, the dosage of pyridostigmine bromide should be adjusted to the minimum dose range that can control symptoms before surgery as far as possible,” the researchers wrote.
A past history of myasthenic crises, seen in about 20% of MG patients, signals the possibility of new severe episodes following surgery, even in patients in whom symptoms were well-controlled before surgery.
“Non-thymoma MG patients should be highly vigilant if combined with the above conditions, take countermeasures in advance, and timely deal with the MG crisis that may occur at any time to ensure the safety of patients,” the researchers wrote.