Dropped head syndrome linked to rare MG with anti-MuSK antibodies
Woman, 64, had muscle weakness in neck, spine
Written by |

A 64-year-old woman with dropped head syndrome was found to have a form of myasthenia gravis (MG) associated with the presence of antibodies against a protein called muscle-specific kinase (MuSK) and axial myopathy, a condition where muscles that protect the spine become weak.
Previous studies have reported axial myopathy associated with dropped head syndrome in MG patients with antibodies targeting acetylcholine receptors (AChRs), the most common type of MG-causing antibodies, or thymomas (tumors in the thymus gland).
This case shows “concurrent axial myopathy in addition to MuSK-MG may have been an underlying factor for [dropped head syndrome] in this case,” according to researchers.
The patient’s case was described in a study, “Dropped head syndrome in anti-MuSK antibody-positive myasthenia gravis with possible concurrent axial myopathy,” published in the journal Clinical & Experimental Neuroimmunology.
Dropped head syndrome commonly caused by MG with anti-AChR antibodies
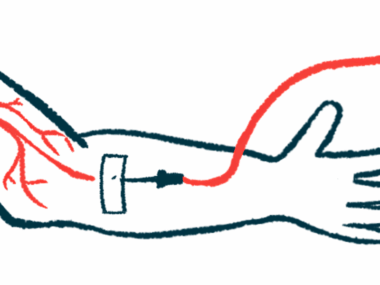
Dropped head syndrome is a group of disorders in which neck muscles become weak and are no longer able to support the head, causing it to bend forward or drop. The condition is commonly caused by MG, an autoimmune condition that affects the neuromuscular junction, which is the site where nerves and muscles communicate to coordinate voluntary movements.
The most common cause of MG is the production of self-reactive antibodies that target AChRs at the neuromuscular junction, although some patients have antibodies targeting other proteins involved in nerve-muscle communication, including MuSK.
Moreover, concurrent axial myopathy, a neuromuscular condition that specifically affects paraspinal muscles — those that help maintain proper posture and protect spinal segments — may also play a role in neck muscle weakness.
However, the presence of axial myopathy occurring in association with dropped head syndrome had been mostly observed in MG patients who were positive for anti-AChR antibodies or in those in whom MG was associated with a thymoma.
Now, researchers in Japan reported the case of a 64-year-old woman with generalized MG who was positive for anti-MuSK antibodies and had dropped head syndrome and a bent spine.
She had a three-month history of dropped head syndrome. A neurological examination revealed neck muscle weakness, eyelid droopiness in both eyes (ptosis), and mild double vision. These observations led doctors to suspect a disorder affecting the neuromuscular junction.
A repetitive nerve stimulation test, which can be used to assess a nerve’s ability to transmit signals to muscles, revealed abnormalities in a range of nerves in the face, neck, shoulder, and arm. These findings, together with other tests, led researchers to suspect MG.
A blood test then revealed the presence of high levels of anti-MuSK antibodies, confirming the diagnosis of generalized MuSK-MG.
Acute and chronic changes in neck and paraspinal muscles
Further tests revealed acute and chronic changes in neck and paraspinal muscles, as well as paraspinal muscle atrophy (wasting). The patient didn’t have autoantibodies associated with inflammatory myopathy, so generalized myopathy was deemed to be unlikely.
“Previously reported cases either had associated thymomas or were positive for anti-AChR antibodies. Our case of MuSK-MG without a thymoma suggests that axial myopathy associated with MG may also be present in thymoma-negative MuSK-MG cases,” according to the researchers.
To control MG, the patient received intravenous immunoglobulin — antibodies obtained from healthy donors that are thought to help neutralize the self-reactive antibodies that drive the disease — for five days. This was followed by treatment with tacrolimus (sold as Prograf, among other brand names) and prednisolone to suppress the activity of the immune system.
Treatment moderately alleviated the woman’s ptosis. Her dropped head syndrome responded minimally to treatment, although it was partially alleviated by adequate neck rest and the use of a neck collar. Her spine curvature did not ease with treatment.
The researchers noted “further investigations are warranted to determine the relationship between axial myopathy and MG.”




Leave a comment
Fill in the required fields to post. Your email address will not be published.