FAQs about Vyvgart
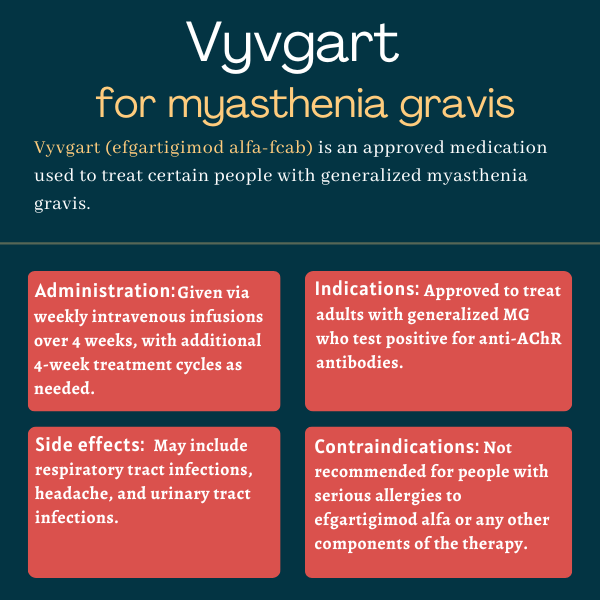
The U.S. Food and Drug Administration (FDA) approved Vyvgart in December 2021 to treat adults with generalized myasthenia gravis (gMG) who are positive for antibodies targeting the acetylcholine receptor. The decision marked the first approval of an FcRn blocker in the U.S. and also made Vyvgart the first approved therapy designed to reduce disease-causing antibodies.
Some generalized myasthenia gravis (gMG) patients may see results as early as two weeks after starting treatment with Vyvgart. The ADAPT+ trial showed that, in adults with gMG, Vyvgart could rapidly improve scores on a patient- and clinician-reported measure of symptom severity within one week. However, as each person is unique and may respond differently to a given treatment, patients should discuss with their healthcare team how Vyvgart may help in their particular case.
There are no clinical data on the use of Vyvgart in pregnant patients. Animal studies found no evidence of a link between the use of Vyvgart and fetal development abnormalities. Patients who are pregnant or are planning to become pregnant should discuss this issue with their healthcare providers.
Vyvgart has been reported to have no or a negligible impact on a person’s ability to drive and use machines. Nevertheless, it’s recommended that patients be careful before attempting to drive or use any machines until they know how Vyvgart affects them. Patients prescribed Vyvgart should talk with their healthcare team regarding the treatment’s potential impact on activities such as driving.
Related Articles

 Fact-checked by
Fact-checked by