Thymoma-associated MG Immune Cell Growth Tied to Parvovirus B19
Infection may cause B-cell proliferation, germinal centers to form
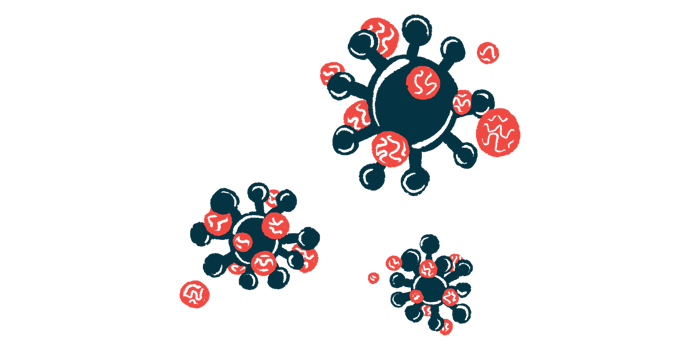
An infection with parvovirus B19 may contribute to abnormal immune cell growth in people who have a thymoma, or thymus tumor, associated with myasthenia gravis (MG), a new study reports.
“This study shows that B19V infection may cause B-cell proliferation and formation of ectopic GCs [germinal centers], subsequently leading to thymoma-associated MG,” the researchers wrote.
The study, “Human Parvovirus B19 May Be a Risk Factor in Myasthenia Gravis with Thymoma,” was published in Annals of Surgical Oncology.
Many people with MG, especially those with early-onset disease, have abnormalities in the thymus, an immune organ in the chest. Abnormal cell growth, or hyperplasia, is common and a subset of patients have a thymoma — a tumor in the thymus gland.
Parvovirus B19, or B19V for short, is well known as the cause of fifth disease, which usually manifests as a mild rash in children. A prior study showed this virus can cause abnormal growth of thymus cells. It’s also been linked to clusters of rapidly growing immune cells, called ectopic germinal centers (GCs), forming in the thymus.
“However, more cases need to be assessed to further elucidate the relationship between this virus and thymoma-associated MG,” the researchers wrote.
To gain more insight into the virus’s role in thymus-associated disorders, particularly MG, researchers in China analyzed surgical samples of the thymus from 708 people with a thymoma.
About one-third (33.2%) of thymoma patients had MG. These patients were on average significantly younger than those without a thymoma. Ectopic GCs were found in 33.6% of cases and significantly more were in patients with MG than without the disease (51.1% vs. 25%).
“These results indicated that both MG and GCs primarily occurred among thymoma patients aged [less than] 50 years and that MG was associated with presence of ectopic GCs,” the researchers wrote, noting their finding is in line with other research that suggests “the presence of ectopic GCs may contribute to the occurrence of thymoma-associated MG.”
Based on DNA testing, B19V was detected in 38 (5.4%) of the 708 thymomas. The rate of B19V positivity was significantly higher among patients with ectopic GCs than in those without them (8.4% vs. 3.8%). However, virus positivity rates did not differ significantly between patients with or without MG, nor did they vary by age or sex.
The researchers also tested for viral proteins, rather than DNA. In these assessments, 19.1% of thymoma samples were positive for B19V, and virus positivity was significantly more common among patients with GCs (24.8% vs. 16.2%) and among those with MG than without (25.1% vs. 16.1%).
These data suggest B19V infection may be linked to developing ectopic GCs, which are themselves linked to thymoma-associated MG.
“To the best of the authors’ knowledge, this is the first report of the presence of B19V in [thymus cells] and ectopic GCs, revealing an unrecognized [disease-causing] mechanism for thymoma-associated MG,” they wrote, adding more research was needed to clear up the “role of B19V in thymic abnormalities with MG.”