Thymectomy eases symptoms in all MG types, study finds
Benefits of thymectomy found in early- and late-onset MG, research indicates
Written by |
People with myasthenia gravis (MG) benefit from thymectomy — surgery to remove the thymus gland — regardless of whether they have early- or late-onset disease or a tumor in the thymus, a study from Germany has found.
The study, “The impact of thymectomy in subgroups of Myasthenia gravis patients: a single center longitudinal observation,” was published in the journal Neurological Research and Practice.
In MG, the body’s immune system mistakenly turns against proteins needed for nerve cells to communicate with muscles. This causes muscles to become weak and easily fatigued over time.
The thymus gland, located in the chest, is home to developing immune cells. Abnormalities in the thymus gland are thought to contribute to the immune attack that drives MG. That’s why surgically removing the thymus gland may help manage MG symptoms.
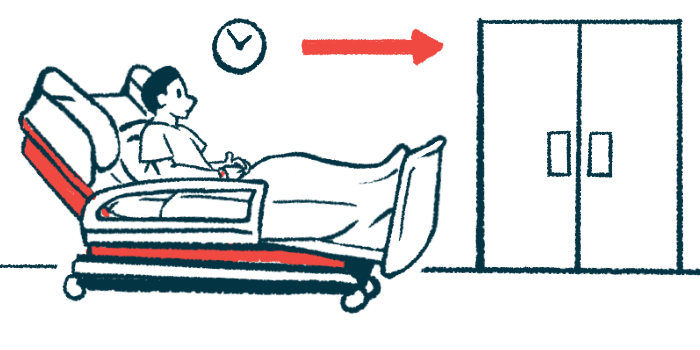
Thymectomy is generally recommended to people with early-onset MG, meaning those in whom the disease begins to manifest at an age younger than 50, who test positive for self-reactive antibodies targeting the acetylcholine receptor — the most common type of MG-causing antibodies. It’s also recommended for those with a thymoma, which is a tumor in the thymus.
Thymectomy studied in all myasthenia gravis types
Researchers in Germany wanted to understand which factors influence the outcomes of thymectomy in order to improve the way patients are treated. To that end, they collected data from an MG center, focusing on adult patients who underwent thymectomy from January 2012 to December 2020.
A total of 94 patients with a mean age of 45.8 years were included in the analyses. More than half (62.8%) were women; 45 (47.9%) had early-onset MG, 28 (29.8%) had late-onset MG, and 21 (22.3%) had thymoma-related MG. Most (78.7%) tested positive for anti-acetylcholine receptor antibodies.
Before surgery, most patients (83.9%) were taking pyridostigmine (sold as Mestinon), whereas others were taking cortisone (72.2%) or another immunosuppressant (28.7%). Thymectomy was done using a minimally invasive approach in 73 patients (77.7%), and sternotomy to access the chest in 21 (22.3%).
People with early-onset MG were on average about 28 years younger than those with late-onset MG (31.1 vs. 59.8 years) and more often were women (75.6% vs. 42.9%). Those with a thymoma had a mean age of 58.6 and almost half (47.6%) underwent sternotomy.
After a median follow-up period of 46 months, researchers found there were no significant differences in quality of life or the ability to carry out activities of daily living among the three groups. There also were no differences in symptom severity.
Complete stable remission
Overall, about one in 10 patients achieved complete stable remission, meaning they had no symptoms of MG for some time and did not take any medication to treat MG during that time.
However, complete stable remission was achieved more frequently among patients with early-onset MG than in those with late-onset MG (18.8% vs. 4.8%). None of the patients with thymoma-related MG achieved complete stable remission.
With thymectomy, it may be possible to lower the dose of cortisone to reduce the risk of long-term side effects. This is called cortisone sparing. Researchers found that thymectomy brought about a reduction of cortisone in both people with early- and late-onset MG, but not in those with a thymoma.
“This study suggests a comparable benefit from thymectomy in terms of symptom control, and cortisone sparing effects, for [early-onset MG] and [late-onset MG] patients,” the researchers wrote.
“Eventually, thymectomy increases the chance of achieving complete clinical remission without ongoing immunosuppressive medication,” they wrote. “We hypothesize that these effects are more generalized in MG patients, beyond the [early-onset MG] subgroup.”






Leave a comment
Fill in the required fields to post. Your email address will not be published.