Low Levels of RNA Molecules in Thymus May Contribute to MG Development
Written by |
An analysis of the thymuses removed from people with myasthenia gravis (MG) found lower levels of micro RNA molecules (miRNAs) that may contribute to disease development by favoring increased production of pro-inflammatory proteins and cells, a study suggests.
In mice, low levels of these miRNAs led to a faster development of complications than those usually seen in MG.
The study, “Decreased expression of miR-29 family associated with autoimmune myasthenia gravis,” was published in the Journal of Neuroinflammation.
In people with MG, antibodies that normally fight off infections mistakingly attack proteins (mainly acetylcholine receptors, AChRs) at the neuromuscular junction — where nerve cell endings connect with the muscles — and impair muscle contraction.
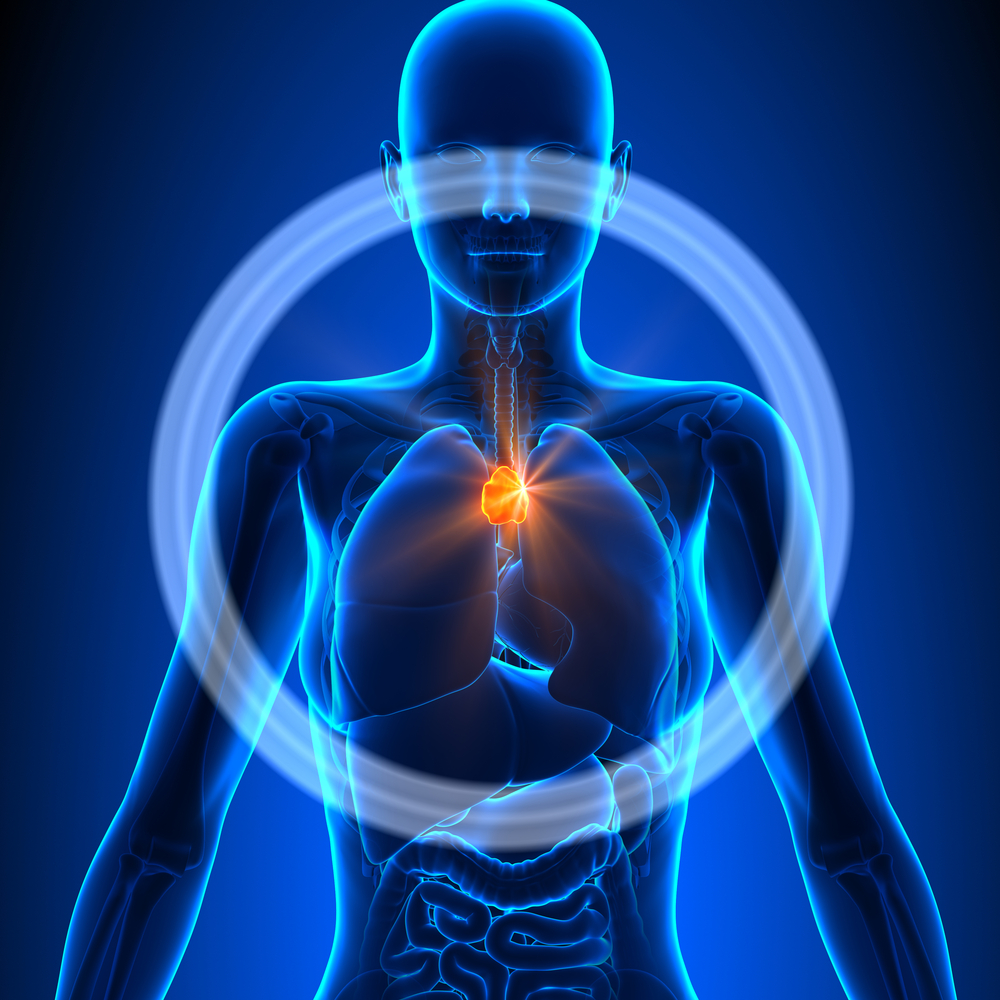
Malfunction of the thymus gland, a specialized organ of the immune system, is associated with MG, and its removal (thymectomy) is a common treatment strategy in MG.
In the early-onset form of MG, the thymus displays abnormalities such as the infiltration of antibody-producing immune B-cells, which leads to overgrowth and production of anti-AChR antibodies.
An excessive activity of genes regulated by interferon (IFN)-beta and IFN-I is observed in the thymus of people with MG. miRNAs are key in regulating gene activity and, in contrast to messenger RNA molecules (mRNA), do not provide instructions to create proteins.
An enzyme called DICER functions to produce miRNAs. Mice lacking this enzyme in cells of the thymus show a buildup of antibody-producing B-cells.
Studies have suggested that a particular family of miRNAs, called miR-29, plays a role in modulating IFN-I signaling.
As such, researchers at the Sorbonne University, in France, and their colleagues investigated the production of DICER and miR-29a in MG patients’ thymuses to further understand the underlying mechanisms of the disorder.
Thymic biopsies from 12 early-onset MG patients (ages 15 to 35) were collected after thymectomy. As controls, the team also analyzed biopsies from six donors without MG and undergoing cardiovascular surgery. Epithelial cells from the thymus were cultured from such donors.
In the thymus of MG patients, the analysis found a 4.6-times decrease in the mRNA of DICER production compared to the controls, which was correlated significantly with a decrease in the mRNA levels of a member of the miR-29a family, called miR-29a-3p.
Further tests confirmed lower levels of almost all miRNAs of the miR-29 family in the thymus of MG patients. A statistical analysis found that these differences were able to distinguish MG patients from controls.
Experiments to determine the cellular source of these differences suggested that the lower levels of miR-29 molecules originated from alterations in epithelial cells of the thymus.
Exposing such cells from healthy donors to IFN-beta induced a lower production of miR-29a-3p, According to the team, this suggests that lower levels of miR-29 subtypes in the thymus could be due to their suppression by IFN-beta in epithelial cells.
To support these results, mice were bred to lower the production of miR-29a as seen in MG patients. The animals were injected with a form of AChR at various body sites to induce complications mimicking MG.
These mice developed symptoms more rapidly than control animals not injected with AChR, especially with reduced amounts of miR-29a. By the end of the experiment, 92% of mice of the MG model were sick, compared to 63% of the controls.
Within the MG model, no differences in anti-AChR antibodies were seen comparing animals with normal or lower levels of miR-29a. According to the scientists, this reveals that the levels of anti-AChR antibodies do not explain the worse symptoms in mice with less miR-29a.
In the thymus, the mRNA of IFN-beta was increased significantly in animals with lower miR-29a levels compared to controls. Likewise, mRNA levels of the immune proteins interleukin (IL)-17a and IL-21 were higher in mice with reduced miR-29a production. This finding suggests a greater amount of Th17 cells, a type of pro-inflammatory immune cell.
“It is not clear if the decreased expression of miR-29 subtypes in human MG is a consequence or a causative factor of thymic inflammation,” the investigators concluded. “However, our results … indicated that a reduction in [mi-R29a] may contribute to … MG by favoring the increased expression of [IFN-beta] and the emergence of pro-inflammatory Th17 cells.”



Leave a comment
Fill in the required fields to post. Your email address will not be published.