Swallowing issues highly common in MG patients: Study review
Dysphagia may be linked to serious complications like lung infections
Written by |
Dysphagia, or difficulty swallowing, is highly prevalent in people with myasthenia gravis (MG) and may be associated with severe complications, including lung infections caused by food aspiration into the airways.
That is according to a review of studies assessing dysphagia in MG patients using objective instrumental tests and subjective scores of disease severity and swallowing outcomes.
“The high prevalence of dysphagia in MG demonstrates the need for early and routine swallowing assessments, particularly using objective instrumental assessment tools,” researchers wrote. “Timely identification and management of dysphagia are critical to preventing serious complications.”
The study, “Swallowing Impairments in Patients with Myasthenia Gravis: A Scoping Review,” was published in Dysphagia by a team of four researchers in the U.S.
Dysphagia reported in up to 70% of MG patients
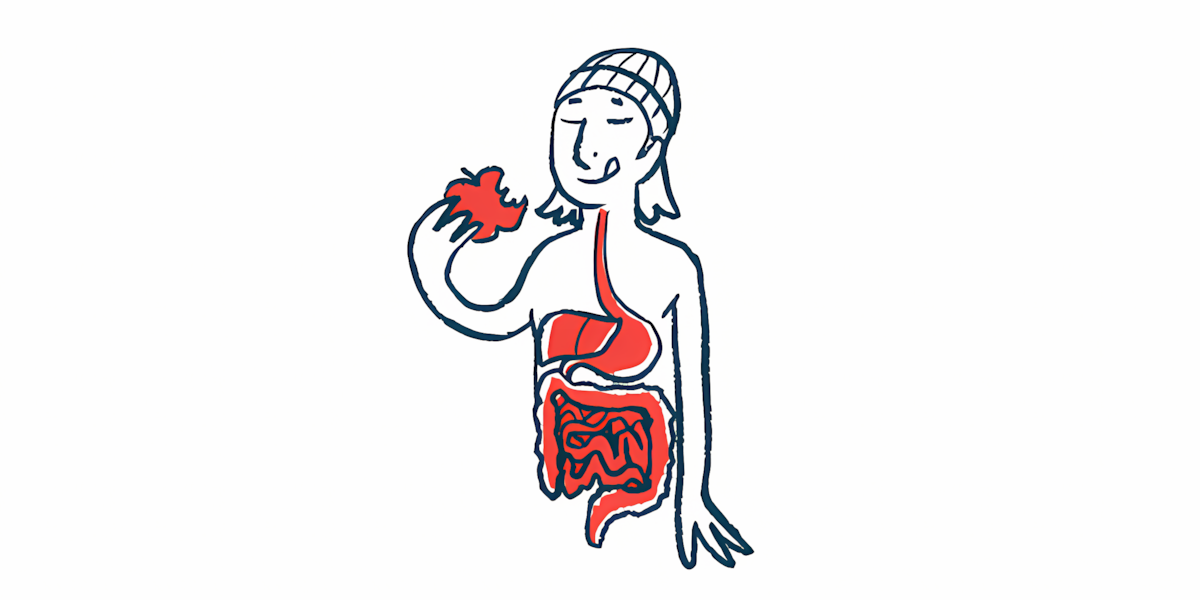
MG is typically caused by self-reactive antibodies that target proteins involved in nerve-muscle communication, resulting in symptoms such as muscle weakness and fatigue. Patients may experience dysphagia due to weakness in the muscles of the mouth, jaw, and tongue.
Dysphagia, which has been reported in up to 70% of MG patients, can lead to severe complications, including silent aspiration, when food or liquid enters the airways without noticeable symptoms.
This increases the risk of aspiration pneumonia, a severe lung infection, and myasthenic crisis, a potentially life-threatening complication that occurs when respiratory muscles become too weak, leading to breathing issues.
“Despite this, much of the current research focuses on generalized muscle weakness, with limited emphasis on swallowing dysfunction,” the researchers wrote. “The prevalence of silent aspiration and the characteristics of swallowing impairments across the oral, pharyngeal, and esophageal domains are not well defined.”
The pharynx refers to the throat, and the esophagus to the tube that carries food from the throat to the stomach.
Swallowing issues frequently reported at the mouth level
In this study, the team systematically reviewed studies published up to March 2025 that reported on the characteristics of swallowing impairments in people with MG. A total of 13 studies, covering 278 patients, were included in the final analysis.
Objective measures of dysphagia included the videofluoroscopic swallowing study (VFSS), an X-ray test used to visualize the food journey from mouth to stomach; fiberoptic endoscopic evaluation of swallowing, where a flexible tube is inserted through the nose to visualize the throat; and esophageal manometry, when a flexible tube with pressure sensors is used to measure the function of esophageal muscles.
Three studies were conducted in Japan and three in Turkey, while the others were conducted in Canada, Germany, the U.S., Brazil, and Taiwan. Two studies compared people with MG with healthy controls, while others compared MG patients with people with neuromuscular disorders.
Pooled results indicated that MG-related dysphagia affects all domains in the swallowing process.
Dysphagia was frequently reported at the mouth level, manifesting as difficulties with the formation and transport of the food ball, or bolus. In one study, issues with bolus transport were reported in 60.8% of the patients. These symptoms typically worsen with fatigue.
Impairments at the pharynx level were highly prevalent and often more severe than oral difficulties. One study reported that all patients with bulbar dysfunction, or weakness in the muscles in the face, tongue, throat, and/jaw, had pharyngeal issues.
The most frequent signs were reduced pharyngeal movements due to muscle weakness and reduced coordination, resulting in impaired pharyngeal contraction and reduced elevation of the larynx, or voice box. Elevation of the larynx is one of the mechanisms used by the body to prevent food from entering the airways during swallowing.
Standard MG severity measures insufficient at detecting impairments
One study identified reduced larynx elevation in 39.1% of VFSS tests, which was significantly associated with an increased risk of aspiration. Several studies indicated a relatively high rate of silent aspiration, and in one study, “75% of the patients with silent aspiration developed aspiration pneumonia during follow-up,” the team wrote.
Dysfunction of the esophagus was frequently reported in MG patients, even in the absence of dysphagia. Studies also indicated that throat issues were associated with delayed transport of the food bolus through the esophagus.
Overall, the studies demonstrated that standard MG severity measures, including Quantitative Myasthenia Gravis and the Myasthenia Gravis Activities of Daily Living, as well as patient-reported outcomes, are insufficient to detect swallowing impairments in people with MG.
Dysphagia screening should not rely solely on overall MG severity. Future research should focus on standardizing dysphagia screening and assessment tools for MG
However, analysis of classification systems used to assess MG severity, including Myasthenia Gravis Foundation of America and Osserman’s Classification, suggested that patients with more severe disease, particularly those with involvement of the mouth, throat, and respiratory muscles, were more prone to swallowing dysfunction and aspiration issues than those with milder disease.
Overall, the results demonstrated that swallowing impairments are prevalent in MG patients, and their severity is often associated with the overall disease severity.
However, classification systems “are inherently subjective,” the researchers wrote, highlighting “the need for more specific and objective measures” that “should be integrated into routine clinical assessments.”
“Dysphagia screening should not rely solely on overall MG severity,” the team concluded. “Future research should focus on standardizing dysphagia screening and assessment tools for MG.”


Bruce Guercio
I was initially, very excited to see this article’s title, as it focused on one of my specific areas of trouble. Unfortunately, I became disappointed when I realized there were several important factors that were overlooked, whether intentional or inadvertently.
First, let me explain my disappointment. I was diagnosed in 2012 with MG, but only after almost a year and half of multiple tests and medication and research. My major symptoms were, swallowing difficultly with choking issues. I began loosing weight very fast and I could only sip light liquids. I did have the “Swallowing X-Ray Test” even went through an esophagus stretching. Either no help.
I was also having trouble talking, especially after talking for awhile, my voice would become a whisper and some words were very difficult to say. This was very frustrating since my whole life I used my voice in public speaking, narrations and leading bible studies.
That was one of my disappointments with this article. No mention of trouble speaking.
Another thing that was missing was a medical procedure to aid with the swallowing problem. Like I mentioned, I would sometimes choke on foods, so I would just not eat. Which of course was not healthy or medically sound due to the lack of nutrition and hydration. After I suffered a broken neck in 2024, I required neck surgery to put in rods to close and support the C-5 vertebra. I was also having a lot of difficulty swallowing my medications. During my ICU & surgery, we decided that a PEG Feeding Tube would be most effective and beneficial to elevated my malnutrition and hydration levels. I could not tolerate the nose feeding tube. Not at all. That was a blessing.
I was surprised how the Feeding Tube is not discussed more often.
I apologize for this being so long, but I do feel very strongly about these issues. For years, my PCP and I we’re going at my medical treatment as if we were blind. Even two Neurologists never suggested a feeding tube.
Thank you for listening to my rant.
Have a blessed day.
Jodi Enders
Bruce, thank you for taking the time to share your experience and for explaining where the article felt incomplete to you. We're sorry for how challenging and prolonged your journey with swallowing, nutrition, and voice changes has been.
The article was based on a news coverage review of a study that focused specifically on swallowing impairments in MG using medical test assessments that directly measure how swallowing works, such as VFSS and endoscopic evaluations. For that reason, it centered on dysphagia across the oral, pharyngeal, and esophageal phases of swallowing and related risks like silent aspiration and lung infections.
You raise an important point about speech and voice difficulties. While these symptoms are often related to bulbar involvement in MG, they were outside the research objective of this particular review, which is likely why they were not addressed by the researchers. We appreciate you sharing your experience and thoughts with us about where broader discussion and research are important.
-Jodi, Patient Advocate