Study Details Clinical Course of Anti-MuSK-positive MG
Written by |

Many people with myasthenia gravis (MG) caused by antibodies against MuSK initially present with eye-related symptoms, which soon affect other parts of the body, according to a new study.
“The present study provides a better understanding of MuSK-MG disease and its clinical course,” its researchers wrote.
The study, “Spotlight on MuSK positive myasthenia gravis: clinical characteristics, treatment and outcomes,” was published in the journal BMC Neurology.
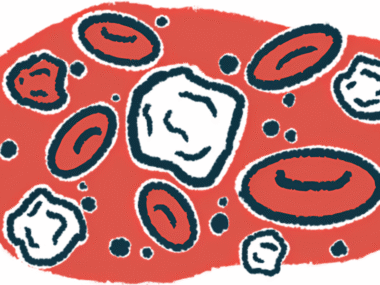
MG is caused by antibodies that interfere with the communication between nerve and muscle cells. In most cases, MG-causing antibodies specifically target a protein called acetylcholine receptor, but more rarely, antibodies targeting another protein called muscle-specific kinase (MuSK) cause MG.
In this study, a trio of scientists in China reviewed data from 21 people with MG caused by anti-MuSK antibodies who were treated at their center over the past decade.
“We systematically reviewed 21 patients diagnosed with MuSK-MG in our centre, and the detailed clinical characteristics, including therapy and disease progression time, were recorded,” the team wrote.
Most patients (81%) were female. The average age at disease onset was just less than 52 years, and the median follow-up time was a little more than three years.
Nearly half of the patients (47.6%) were diagnosed initially with ocular MG, with symptoms mainly affecting the eyes, such as double vision or drooping eyelids. Almost 43% had bulbar MG, where muscles in the mouth and throat are the ones most affected, causing speech impairment, difficulties swallowing and breathing. The remaining 9.5% had generalized MG, which affects muscles throughout the body.
Of note, over the course of follow-up, all the patients who originally had ocular MG progressed to having generalized MG. The average time to progression was just over four months.
Six of the 21 patients experienced an MG crisis — a potential life-threatening episode in which muscles involved in breathing become affected. The median time from disease onset to MG crisis was 7.76 months.
For treatment, 81% of the patients received pyridostigmine (sold as Mestinon, among other brand names), and more than 90% were given corticosteroids or other immune-suppressing medicines. Other treatments also were used, but less commonly. Most patients received more than one medication over the course of their treatment.
Researchers highlighted that at the end of follow-up three patients were being treated with traditional Chinese herbal remedies, and those three patients had generally stable symptoms with this treatment.
Long-term follow-up data were available for 18 of the 21 patients. Outcomes were generally good: one patient was in complete remission, 42.9% had minimal manifestations of the disease, 19% experienced an improvement in their condition, and one patient’s clinical status remained largely unchanged. Two patients died from MG-related complications over the course of follow-up — a 72-year-old man and a 58-year-old woman.
“The use of combination treatment might be helpful for symptom improvement and clinical outcome,” the researchers wrote. “However, some patients with MuSK [antibodies] responded poorly to standard care. Therefore, early introduction of more effective treatments should be considered once a diagnosis is confirmed.”

Leave a comment
Fill in the required fields to post. Your email address will not be published.