Novel system may predict outcomes in MG linked to thymus tumor
Study proposes use of 2 standardized assessment tools for better classification
Written by |
Using a combination of two standardized assessment tools may be better than the classification process now in place in predicting the outcomes of people with a thymoma, or thymus tumor, associated with myasthenia gravis (MG), a new study suggests.
The newly proposed system, from researchers in China, would classify patients based on a combination of the Myasthenia Gravis Foundation of America (MGFA) classification system — an assessment of MG severity — and the Masaoka staging for tumor invasiveness measure.
Compared with either MGFA or Masaoka alone, this new system for classifying thymoma-associated myasthenia gravis, or TAMG, more accurately predicts outcomes related to remission, MG complications, tumor surgery, and survival, according to the researchers.
“This novel TAMG classification provides valuable information on outcome stratification and clinical decision-making for TAMG,” the team wrote.
Their study, “A new pragmatic classification system for thymoma associated myasthenia gravis: a retrospective cohort study,” was published in the International Journal of Surgery.
Researchers call classification systems in use ‘insufficient’
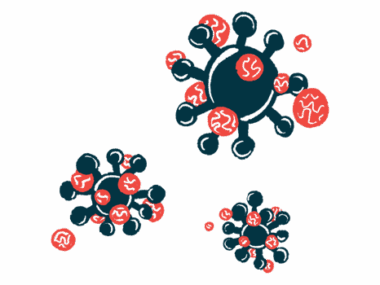
MG is an autoimmune disorder in which self-reactive antibodies damage components of the neuromuscular junction, where nerves connect to muscles to coordinate voluntary movements. This results in symptoms of muscle weakness and fatigue that worsen with exercise.
Why these self-reactive antibodies are produced in MG is not well established, but abnormalities in the thymus gland, an organ in the upper chest that produces T-cells for the immune system, are thought to play a role.
About 15% of MG patients have thymomas, while approximately 35% of people with a thymus tumor have MG, according to the researchers. Surgery to remove the thymus, called a thymectomy, is typically recommended for TAMG patients. However, because TAMG can manifest with both tumor and MG symptoms, treatment approaches may differ from those used for each condition alone.
In people with MG or a thymoma alone, clinicians rely on staging systems that assess disease severity to determine the best treatment approach. In particular, the Masaoka staging is used for gauging tumor invasion — classified as stages I-IV — and the MGFA classification system, using class 1-5, assesses the severity of MG.
According to researchers in Shanghai, however, “relying solely on Masaoka staging or MGFA classification to determine the treatment approach and predict postoperative outcomes is insufficient.”
New classification system proposed for patients with thymus tumor
To address this gap, the team, from Zhongshan Hospital and Fudan University, proposed a novel TAMG classification system that combines both Masaoka staging and MGFA. The goal was to help guide surgical decisions and management for these patients.
Using data from 253 people with TAMG who underwent total thymectomy from 2006 to 2022 at their hospital, the team classified patients into four novel types of TAMG.
Type A, which comprised 104 cases (41.1%), was defined as Masaoka stage I-II (non or minimally invasive tumor) and MGFA class 1 (eye muscle weakness only). Type B consisted of 59 patients (23.3%) with Masaoka stage III-IV (tumor growing into nearby tissues or beyond) and MGFA class 1, or with Masaoka stage I-II and MGFA class 2 (mild weakness affecting muscles beyond eye muscles).
In type C, 72 patients (28.5%) had Masaoka stage III-IV and MGFA class 2 or stage I-II and MGFA class 3-4 (moderate to severe muscle weakness). The most severe, type D, with 18 cases (7.1%), was defined as Masaoka stage III-IV and MGFA 3-4.
Overall, this four-class classification system improves survival stratification, predictability of myasthenic remission, and the occurrence of [myasthenia crisis]. … [The findings may help] guide surgical decisions and perioperative management for patients.
When matched with clinical data, type A patients had the highest MG symptom remission rates at one, three, five, and 10 years, while type D had the worst remission rates. Although all three assessment systems were good indicators of MG symptom relapse, the TAMG classification had a better predictive value, the data showed.
Similar results were observed for overall survival, with significant differences between types A and types C and D. In comparison, only Masaoka stage IV versus stage I, and MGFA class 2-3 versus class 1, reached significant differences. The TAMG classification system also predicted survival better than either Masaoka or MGFA alone.
A surgical outcomes analysis revealed that type A patients had the best MG activities of daily living scores, while type C and D patients had significantly longer hospital stays compared with those from type A.
Type D patients also had a higher rate of post-thymectomy myasthenia crisis (66.7%), marked by breathing difficulties that usually require hospitalization and ventilation support. Type C patients had the second highest rate, at 22.2%. In contrast, patients from MGFA class 4 had the highest occurrence of myasthenia crisis (52.6%), followed by class 3 (18.5%). Class 2 also had a relatively high rate, at 15.5%.
“Overall, this four-class classification system improves survival stratification, predictability of myasthenic remission, and the occurrence of [myasthenia crisis],” the researchers wrote, adding that these findings may help “guide surgical decisions and perioperative management for patients with TAMG.”

Leave a comment
Fill in the required fields to post. Your email address will not be published.