Myasthenia Gravis Patients’ Gut Microbiome Less Diverse, More Pro-Inflammatory, Study Shows
Written by |
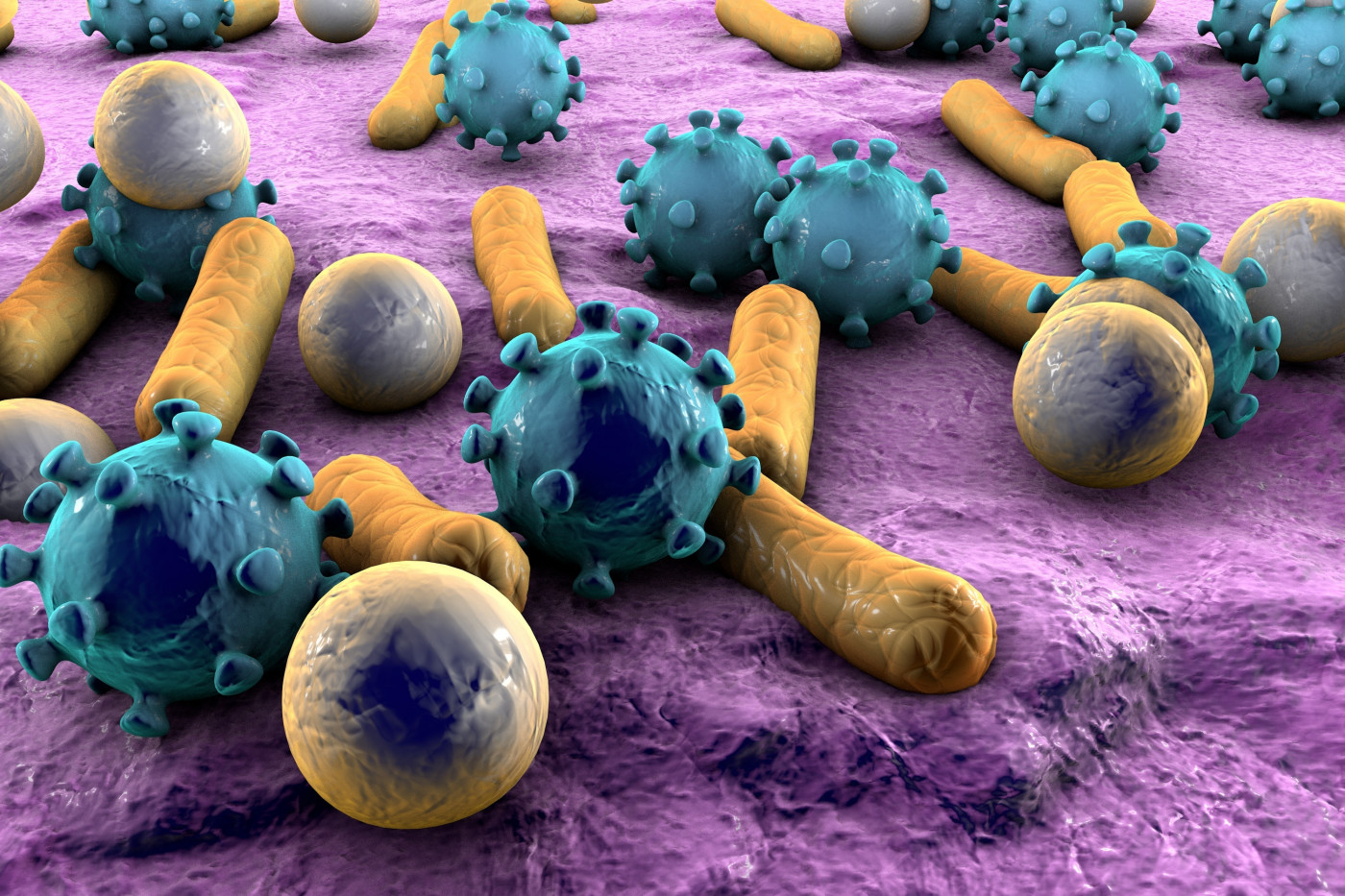
The gut microbiome of people with myasthenia gravis is less diverse than that of healthy people, with a rise in pro-inflammatory bacteria and a reduction in protective molecules, a new study shows.
The study, “Altered Gut Microbiota in Myasthenia Gravis,” was published in the journal Frontiers in Microbiology.
The underlying cause of myasthenia gravis, an autoimmune disorder, is unclear. However, both genetic and environmental factors are in play.
Increasing evidence suggests that the gut microbiome — the collection of natural microbes living in our guts — is able to regulate the immune system and has been shown to play a role in other autoimmune diseases, like systemic lupus erythematosus or inflammatory bowel disease.
However, gut microbiome’s role in myasthenia gravis remains largely unknown.
In this study, a team of researchers compared the gut microbiome of 53 patients (31 men and 22 women) with myasthenia gravis (median age 43.6 years) to that of 50 age- and sex-matched healthy controls recruited at a hospital in China.
The gut microbiome content of the participants’ feces was analyzed.
The majority of patients (35) had ocular myasthenia gravis and the remaining generalized disease with scores in the quantitative myasthenia gravis (QMG) scale — used to measure disease severity — varying from 5 to 13 (ocular disease) and from 8 to 16 (generalized disease). The higher the scores, the more severe the disease.
Patients were analyzed during a period of symptom stability as shown by no changes in their muscle weakness and abnormal fatigability in the QMG scale.
The results showed that the content of the gut microbiome is different between myasthenia gravis patients and healthy controls.
Specifically, the analysis showed that microbial diversity was significantly reduced in the microbiome of patients relative to controls, particularly for members of the phylum Firmicutes, including bacteria of the genus Lactobacillus and Clostridium. Clostridium was approximately three times more abundant in healthy controls.
On the contrary, the abundance of bacteria from the phylum Proteobacteria and Bacteroidetes was significantly higher in myasthenia gravis patients.
Changes in the Firmicutes/Bacteroidetes ratio is linked with a more pro-inflammatory environment and has been found in IBD.
“These findings lend support to the notion that changes in the F/B [Firmicutes/ Bacteroidetes] ratio are linked to a range of autoimmune- mediated disorders,” like myasthenia gravis, researchers wrote.
Researchers also looked at the levels of short-chain fatty acids, or SCFAs, metabolites produced by microbes and known for their beneficial properties for the gut. For example, butyrate is a key component for colon health, with anti-carcinogenic and anti-inflammatory properties.
Moreover, SCFAs promote healing and regeneration of the intestinal epithelium and stimulate the growth of beneficial gut microbes.
The results revealed that SCFAs were lower in myasthenia gravis patients, which is in agreement with the lower abundance of Clostridium, one of themain producers of SCFAs.
Deficiency in SCFAs also is linked with a lower abundance of a group of regulatory T-cells, those involved in keeping the immune system in check.
The alterations in the gut microbiome, called dysbiosis, correlated with the levels of inflammatory biomarkers in the blood of myasthenia gravis patients.
Overall, “our results provide the first evidence that MG [myasthenia gravis] disease features a dysbiotic microbiota with an overall depletion of microbial diversity, as well as an altered structure of the microbial community,” the study concluded.
Leave a comment
Fill in the required fields to post. Your email address will not be published.