Patient with Three MG Antibodies Described in Case Report
A patient with three different types of myasthenia gravis (MG)-associated antibodies was described in a recent case report.
The report, “Anti-MuSK positive myasthenia gravis with anti-Lrp4 and anti-titin antibodies,” was published in Internal Medicine.
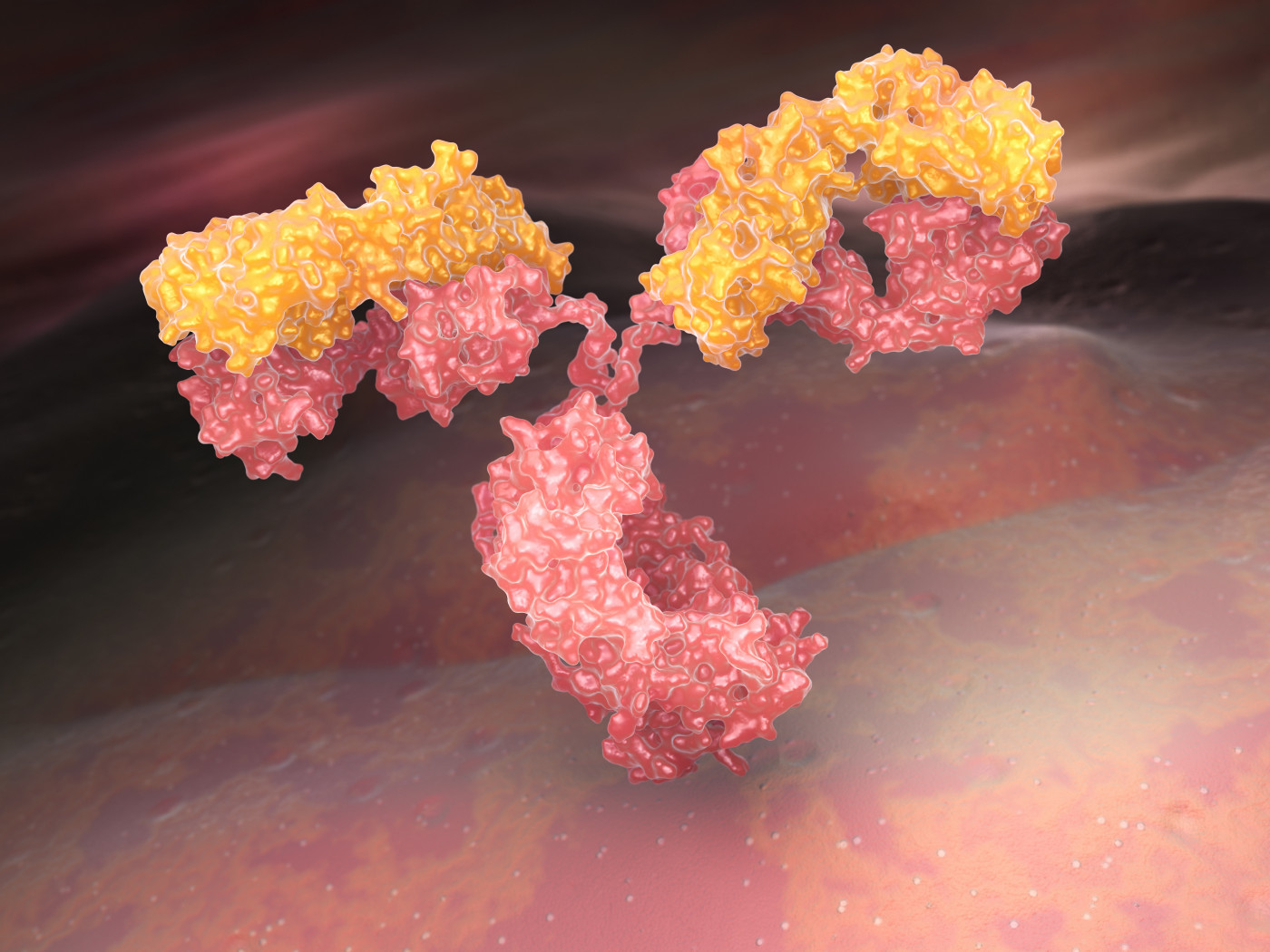
MG is caused by the immune system attacking the neuromuscular junction (NMJ), which is where nerve cells intersect and communicate with muscle cells. This usually is the result of antibodies that wrongly target NMJ proteins.
Specifically, about 80% cases of MG are associated with antibodies against acetylcholine receptor (AChR), a protein that is integral in nerve-muscle communication. Antibodies against muscle-specific kinase (MuSK), another protein involved in this communication, account for most cases of MG where there are no anti-AChR antibodies.
Antibodies against other NMJ- or muscle-associated proteins have been described in MG, but because they are comparatively rare, little is known about the role they play in disease.
In the new report, researchers in Japan described the case of a 62-year-old woman who was brought to the hospital after losing consciousness. Over the decade prior, the patient had experienced intermittent double vision, ptosis (drooping eyelids), and dropped head.
Upon arriving at the hospital, the patient was not breathing, necessitating the use of an artificial ventilator.
A variety of assessments and diagnostic tests were performed. Neurological examination revealed weakness in the muscles of the patient’s face and neck — including difficulty swallowing — and a muscle biopsy revealed muscle atrophy (shrinkage) without inflammation. Other examinations, including an assessment of heart function, were generally within normal ranges.
Further laboratory tests confirmed the presence of anti-MuSK antibodies in the patient’s blood.
In addition, antibodies against two other noteworthy proteins — low-density lipoprotein receptor-antigen (Lrp4), and titin — were identified. Lrp4 is involved in NMJ signaling, whereas titin is a structural protein in muscle cells themselves. Antibodies against both proteins have been associated with MG, though they are comparatively rare, and the combination of all three antibodies has not been documented previously.
“To the best of our knowledge, this is the first detailed report of a case with triple antibody positive MuSK MG,” the researchers wrote.
The patient was treated first with high-dose steroids (methylprednisolone) in combination with tacrolimus, an immunosuppressive medication.
“Her respiratory function gradually recovered after the first steroid pulse therapy, and ventilator support was thereafter completely removed,” the researchers wrote.
Subsequently, the patient was switched to maintenance treatment with the immune-suppressing medicine cyclosporine, in addition to pyridostigmine, a muscle strengthener.
The patient gradually regained the ability to swallow by about two months after the initial hospital admission, and was discharged shortly thereafter.
While it is impossible to draw broad conclusions from a single case study, this report adds to the growing body of literature describing comparatively rare MG-associated antibodies. For example, previous research has suggested that the presence of both anti-MuSK and anti-Lrp4 antibodies is indicative of more severe disease, which tends to respond well to immune-suppressing therapies.
“Consistent with the previous cohort study, our patient showed MG crisis with severe bulbar symptoms, which effectively responded to high-dose steroid and oral immunosuppressive therapy,” the researchers wrote.
The presence of anti-titin antibodies is noteworthy for two main reasons. First, it suggests that the immune system is attacking not just the NMJ, but the muscle cells themselves. Second, while anti-titin antibodies have been previously reported in MG, they almost always appear alongside anti-AChR antibodies, which were absent in this patient.
“Thus, our case further supports the previous observation that anti-titin Abs [antibodies] occasionally coexist with antiAChR negative MG,” the researchers wrote.






