Mitochondria Defects in Immune Cells May Cause MG, Study Says
Written by |
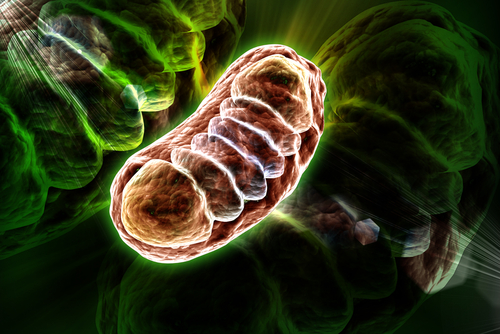
Defects in mitophagy — the process that degrades defective mitochondria, the cell compartments responsible for producing energy — in certain types of immune cells may cause myasthenia gravis (MG), a study contends.
The findings also suggest that an antibiotic with immunosuppressant properties, called rapamycin, holds promise as an MG treatment.
The study, “Effects of Mitophagy on Regulatory T Cell Function in Patients With Myasthenia Gravis,” was published in the journal Frontiers in Neurology.
MG is caused by the production of harmful antibodies that wrongly target proteins required for muscle contraction.
As in other autoimmune disorders, the production of autoantibodies in MG stems from an imbalance in the levels of pro- and anti-inflammatory immune cells.
“At present, it is believed that the abnormal number or function of [regulatory T-cells] may be the trigger point for MG,” researchers wrote.
Regulatory T-cells, or Tregs, are a subtype of immune T-cells responsible for controlling the activity of other types of immune cells. More specifically, Tregs normally are activated to lower the activity of pro-inflammatory immune cells, in order to reduce tissue inflammation.
Mitochondrial impairments and defects in mitophagy — a form of autophagy — have been associated with T-cell malfunction and death.
Such observations led researchers at Hubei University of Medicine, in China, to wonder if Treg defects in MG patients could be caused by problems in mitophagy and mitochondria.
To investigate the hypothesis, they collected blood samples from 15 MG patients and 15 healthy individuals (controls) to isolate Tregs.
In lab-cultured Tregs from patients, the scientists used two pharmacological agents — rapamycin to promote mitophagy, and 3-methyladenine (3-MA) to block this process. Rapamycin, marketed as Sirolimus, is used to prevent rejection of kidney transplants.
The investigators then compared mitophagy levels by examining mitochondria inside Tregs using high-resolution microscopy.
Mitochondria function — assessed by examining the membrane potential — and Tregs’ ability to suppress the proliferation of pro-inflammatory T-cells were both assessed by an approach called flow cytometry.
Notably, mitochondrial membrane potential refers to the difference in electrical charge between mitochondria’s inner and outer membrane and is the driving force for the production of energy. Lower membrane potential is usually an indicator of mitochondria impairment and is one of the factors that induces mitophagy.
Results showed that the levels of mitophagy were lower in patient-derived Tregs compared to controls.
Rapamycin led to higher mitophagy levels than in untreated cells from the MG group. In contrast, 3-MA resulted in lower levels.
Additional lab tests also showed that the levels of LC3-II, a protein involved in autophagy, were lower in patients than in controls. Autophagy is the process by which cells degrade or recycle components that are damaged or no longer needed.
As previously seen with mitophagy levels, LC3-II in untreated Tregs from patients was lower than in rapamycin-treated cells and higher than in 3-MA-treated cells.
The team also found that Tregs from patients were less capable of preventing the proliferation of pro-inflammatory T-cells compared to Tregs from healthy individuals. In addition, mitochondria from patients had lower membrane potential, which indicates dysfunction.
However, the scientists also observed that the membrane potential of mitochondria from patients could be increased with rapamycin to enhance mitophagy. Treatment with rapamycin also increased Tregs’ ability to suppress T-cell proliferation.
According to the team, the findings “reveal the possible cellular immune mechanism of Treg dysfunction in MG,” and suggest that rapamycin “can be used to treat patients with MG.”
Yet, they also added that additional studies are needed to pinpoint the exact mechanisms by which rapamycin exerts these effects.



Leave a comment
Fill in the required fields to post. Your email address will not be published.