IL-23/Th17 Cell Pathway May Be New Target to Control Inflammation in MG Patients, Study Shows
A team of French researchers may have found a new therapeutic target, the IL-23/Th17 signaling cascade, to control tissue inflammation in patients with myasthenia gravis.
The study, “Il-23/Th17 cell pathway: A promising target to alleviate thymic inflammation maintenance in myasthenia gravis,” was published in the Journal of Autoimmunity.
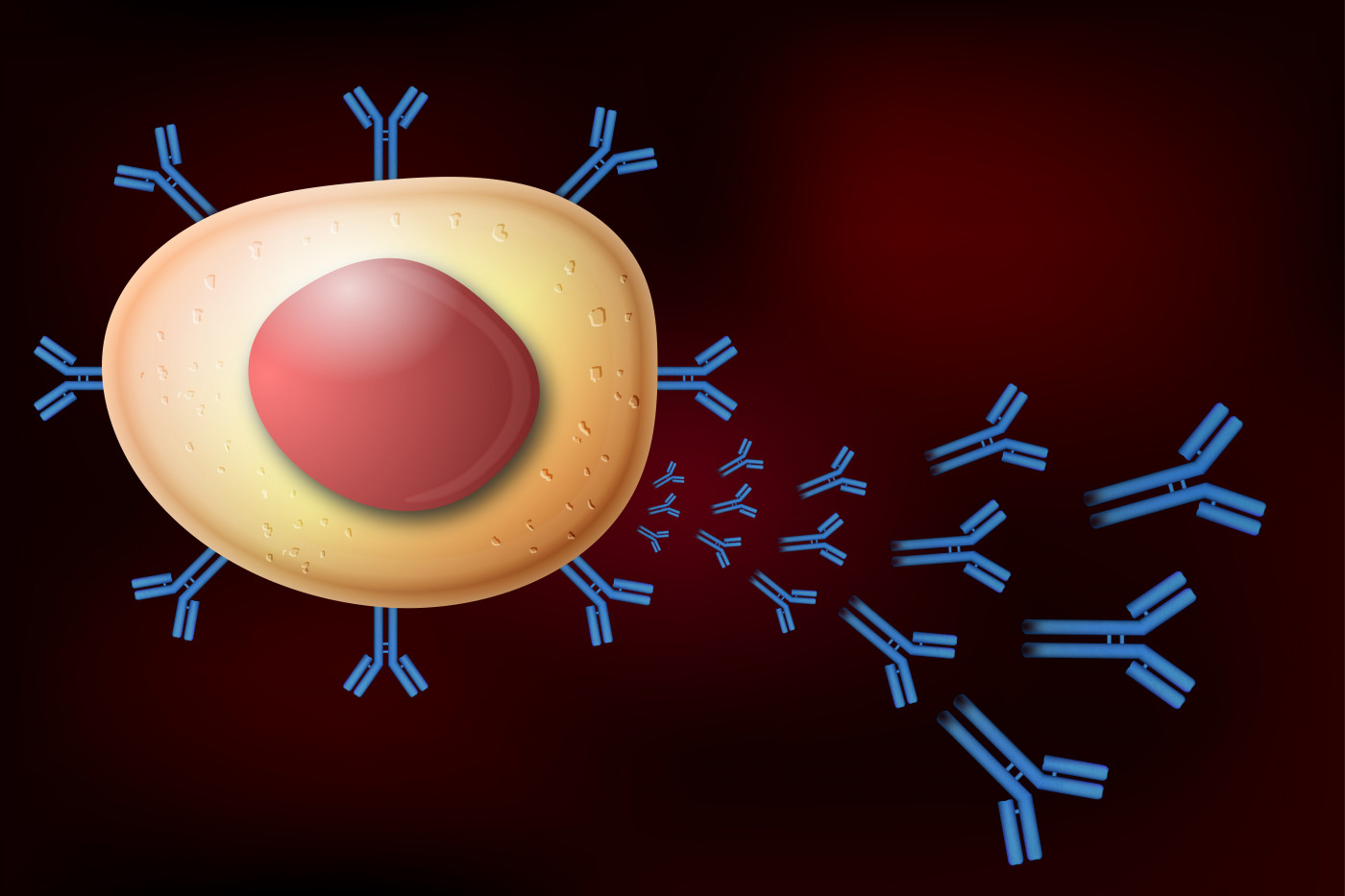
Myasthenia gravis (MG) is an autoimmune disorder caused by the abnormal production of antibodies against acetylcholine receptors (AChR) that are necessary for muscle contraction.
In other types of autoimmune diseases, the IL-23/Th17 signaling pathway has been shown to promote and sustain tissue inflammation. For this reason, medications that target and block components of this signaling pathway have already been developed and approved for the treatment of inflammation.
“To date, monoclonal antibodies anti-IL-23 (interleukin-23) (such as ustekinumab, which is sold by Janssen under the brand name Stelara) are already approved by FDA (U.S. Food and Drug Administration) and are used to treat patients affected with Crohn’s disease and psoriatic arthritis. Therefore, we consider that targeting IL-23 in AChR+ MG could decrease . . . inflammation and antibody production (in MG),” the researchers said.
To explore this idea, researchers at the Sorbonne Université and collaborators set out to characterize the molecular and cellular components involved in tissue inflammation in MG patients.
They analyzed biopsies of the thymus — the gland that produces T-cells, the killers in our immune system — from 51 non-MG controls undergoing cardiovascular surgery, and 72 MG patients undergoing thymectomy (surgical removal of the thymus).
Molecular analyses showed that thymuses from MG patients produced excessive amounts of interleukin-17 (IL-17) — a cytokine (a molecule that mediates and regulates immune and inflammatory response) associated with T-helper 17 (Th17) cells activation — compared with controls. T-helper cells are a sub-type of T-cells that are responsible for regulating the function of other types of immune cells, such as B-cells and killer T-cells.
In addition, data revealed that epithelial cells from the thymus also boosted and sustained Th17 activation by releasing high amounts of another cytokine, called interleukin-23 (IL-23). This over-production of IL-23 was caused by a perturbation in a signaling cascade involving interferon type I (IFN-I) — a class of proteins that regulate the activity of the immune system.
These activated Th17 cells tended to localize around ectopic (abnormal position) germinal centers in the thymus — the region where B-cells grow, differentiate, and produce antibodies — directly influencing B-cells’ maturation and antibody production.
Finally, investigators found that IL-23 production was also boosted by IL-17, which was released by Th17 cells themselves, thereby creating a positive feedback loop of inflammation in the thymus of MG patients.
“Activation of the IL-23/Th17 pathway in the thymus of autoimmune myasthenia gravis patients creates an unstoppable loop of inflammation that may participate in ectopic germinal center maintenance,” the researchers wrote.
They concluded that “targeting IL-23 in AChR+ MG could decrease concomitantly thymic and peripheral inflammation and antibody production. Therefore, IL-23 should be proposed as a new promising therapeutic target in MG.”






