Muscle Regeneration Delayed in Myasthenia Gravis As Stem Cell Functioning Is Impaired, Study Suggests
Muscle regeneration in myasthenia gravis likely is delayed as a result of the impaired functioning of muscle stem cells, called satellite cells (SCs), a study has found.
The study, “Muscle satellite cells are functionally impaired in myasthenia gravis: consequences on muscle regeneration,” was published in the journal Acta Neuropathologica.
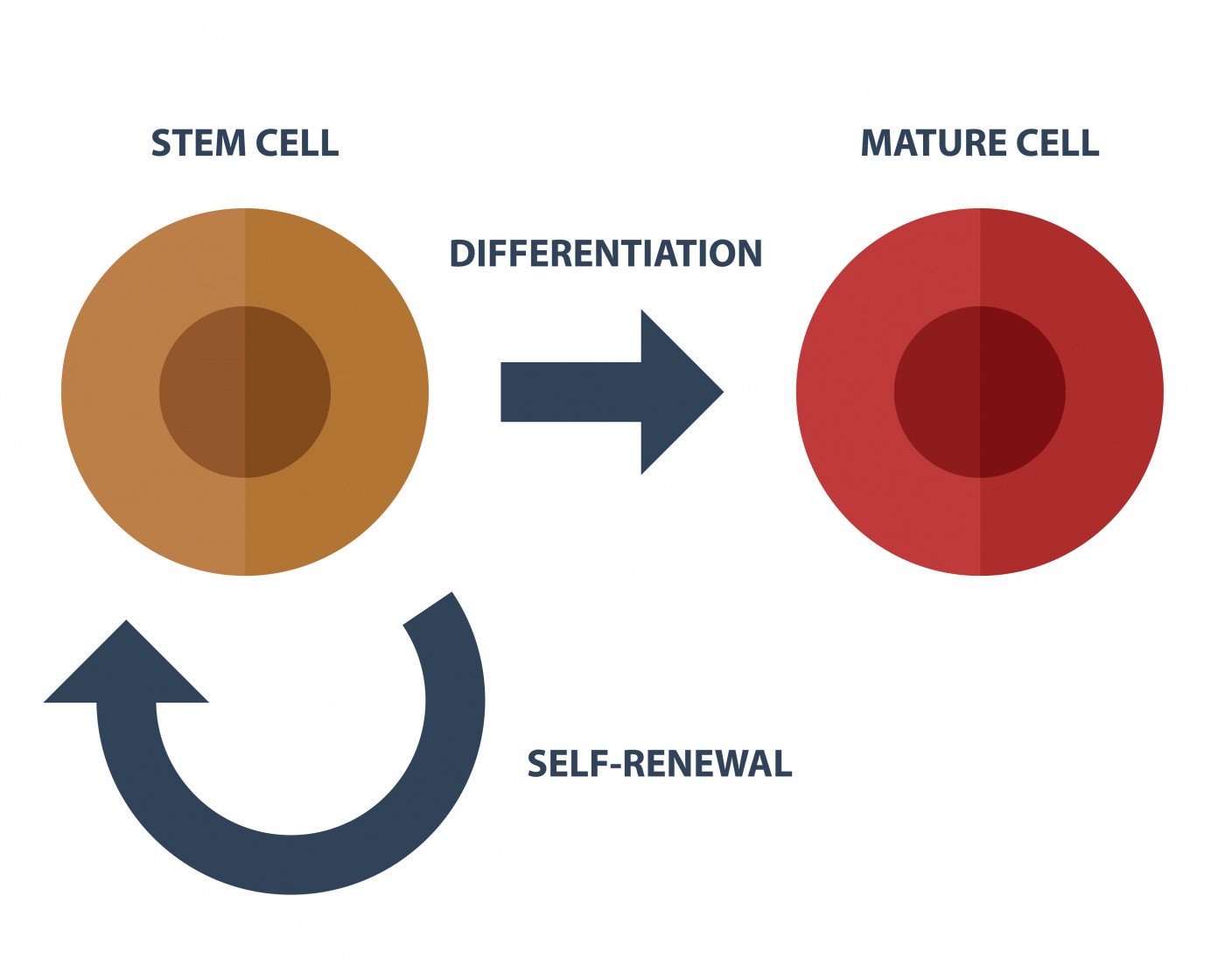
Muscle-specific stem cells, called SCs, are activated and proliferate in order to replenish muscle tissue that is damaged in a process known as myogenesis. The role of SCs in the neuromuscular disease myasthenia gravis, however, had remained unaddressed.
The study’s authors set out to “characterize the functional properties of myasthenic SCs as well as their abilities in muscle regeneration.”
They isolated SCs from muscle biopsies of patients with myasthenia gravis, as well as age-matched controls without myasthenia gravis. Researchers used a specific marker for SCs, called the Pax7+, and observed that the number of SCs is increased in muscle sections from myasthenia gravis patients when compared with aged-matched controls. The increase was also detected in the experimental autoimmune myasthenia gravis (EAMG) mouse model. These results suggest that this cell population is affected in myasthenia gravis.
To determine if the SCs in diseased muscles were still functional, researchers analyzed the muscle sections for expression of two markers (MyoD and Ki67) of SC activity. The results showed that “SCs were more active in myasthenia gravis muscles and displayed higher proliferative rate during myasthenia gravis disease compared to control muscles,” the authors wrote.
Upon isolation of SCs from their muscle environment they become active and are designated as myoblasts. The cells’ proliferation and differentiation profile (their ability to transform into different cell types within the muscle) was more active in myoblasts isolated from myasthenia gravis muscles compared to those in the controls.
The team then performed further experiments to identify factors in myasthenia gravis that may lead to the high proliferation and differentiation rate detected in SCs. The results showed that control myoblasts, when in contact with blood serum from myasthenia gravis patients, exhibited a significant increase in their differentiation rates.
Finally, researchers investigated “whether the main function of SCs, i.e., muscle regeneration, was altered in myasthenic muscles in vivo.” They used the experimental autoimmune myasthenia gravis (EAMG) mouse model and observed that the mice have delayed muscle regeneration in myasthenic skeletal muscle following acute injury.
Overall, these results show that the functioning of the SCs is altered and impaired in the muscles of myasthenia gravis patients.
“The autoimmune attack in MG appears to have unsuspected pathogenic effects on SCs and muscle regeneration, with potential consequences on myogenic signaling pathways, and subsequently on clinical outcome, especially in the case of muscle stress,” the study concluded.






