Blinatumomab helps 2 women with resistant MG: Case report
Cases suggest cancer drug may aid hard-to-treat autoimmune conditions
Written by |

A case report from Germany showed that two women with severe, treatment-resistant myasthenia gravis (MG) responded well to blinatumomab, suggesting the anti-cancer medication may offer a new option for hard-to-treat autoimmune diseases.
“Since this first-in-human experience comprises two cases, our findings should be viewed as proof-of-concept rather than evidence of broad clinical efficacy,” the researchers wrote, noting that further evaluation is needed “to assess the long-term efficacy, safety profiles, and mechanistic pathways of blinatumomab in MG.”
The cases were described in the study, “CD19xCD3 T cell engager blinatumomab effective in refractory generalized myasthenic syndromes,” published in Molecular Therapy.
MG occurs when the immune system produces antibodies that disrupt the communication between nerves and muscles, causing weakness that worsens with activity. While MG treatments exist, some patients don’t respond well; these cases are known as refractory MG.
The two women in the case report had refractory MG that had not improved with multiple treatments.
Improvements in strength, walking ability
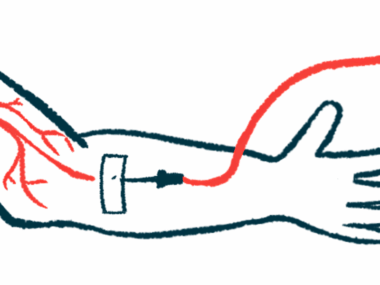
Blinatumomab, marketed under the brand name Blincyto, is normally used to treat leukemia, a type of blood cancer. It works by bringing immune T-cells into close contact with B-cells — the immune cells responsible for producing antibodies — and prompting T-cells to destroy them. It acts faster and more deeply than other B-cell depleting medications, such as rituximab.
The first patient, a 41-year-old woman, was diagnosed with MG in August 2020. She had been treated with a wide range of therapies, including corticosteroids, intravenous immunoglobulins, plasma exchange, rituximab, and newer therapies like Zilbrysq (zilucoplan). Yet she remained severely disabled, struggling with breathing and movement.
The second patient, a 60-year-old woman, was diagnosed with anti-acetylcholine receptor antibody-positive MG in October 2021. She had also been diagnosed with Lambert-Eaton myasthenic syndrome, a related disease. Like the first patient, she had failed to respond to many treatments and had repeated myasthenic crises requiring emergency care.
Each patient received two cycles of blinatumomab through a 12-day continuous intravenous (into-the-vein) infusion, with increasing doses in the second cycle. Other immunosuppressants were paused before the treatment, and both patients received corticosteroids and paracetamol to prevent cytokine release syndrome (CRS), a side effect caused by an overactive immune system.
Both women saw quick and lasting improvements. Scores in scales assessing MG’s impact on daily function (MG Activities of Daily Living, or MG-ADL) and muscle strength (Quantitative MG, or QMG) dropped significantly.
By the end of the first treatment cycle, MG-ADL scores dropped by four points in the first patient and by three in the second. The first patient’s QMG score dropped from 27 to 18 within a month and kept improving over three months. In the second patient, the QMG score dropped from 19 to 8 in the same period and remained stable at 7 points after three months.
These changes were accompanied by other clinical improvements, including in the patients’ ability to walk, as reflected by an increase in step counts tracked by smartwatches.
Blood tests showed different immune responses. In the first patient, B-cell numbers stayed low, consistent with her improvement. In the second patient, B-cell counts rose again after about three months, but her antibody levels continued to fall, and she kept getting better. This could mean the new B-cells weren’t harmful or differed from the disease-causing ones.
One patient also had clear improvements in skin and joint problems associated with autoimmunity, suggesting treatment benefits could extend beyond muscle strength.
Side effects were mild. Both patients experienced CRS, with mild fever, general malaise, and headaches. One patient had temporary diarrhea and reported worsening of pre-existing tachycardia (fast heartbeat) during the first treatment cycle.
Blinatumomab may offer a unique way to treat MG by eliminating long-lived antibody-producing cells that other medications may miss. Unlike rituximab, it doesn’t rely on the body’s natural immune system to kill B-cells. Unlike immune cell therapies, it doesn’t require chemotherapy or months-long preparation, making it more accessible.
However, the report covers only two cases, both women, with a short follow-up period. Their differing types of MG and different treatment histories mean results can’t be generalized. Randomized clinical studies are needed to confirm the treatment’s effects and determine the best dose and schedule, the researchers said.



Leave a comment
Fill in the required fields to post. Your email address will not be published.