Both IVIG and SCIG Effective as Maintenance Therapy in MG, Study Finds
For the first time, a real-world study comparing the effects of long-term intravenous (IVIG) and subcutaneous immunoglobulin (SCIG) maintenance therapy in adults with generalized myasthenia gravis (gMG) showed reduced impairments, less use of other medications, and improved overall health status.
Results also showed that 27 of 30 patients in the study (90%) preferred SCIG after being treated first with IVIG.
The study, “Chronic immunoglobulin maintenance therapy in myasthenia gravis,” was published in the European Journal of Neurology.
MG is an autoimmune disease in which autoantibodies attack the neuromuscular junction — where nerve cell endings connect and communicate with muscles.
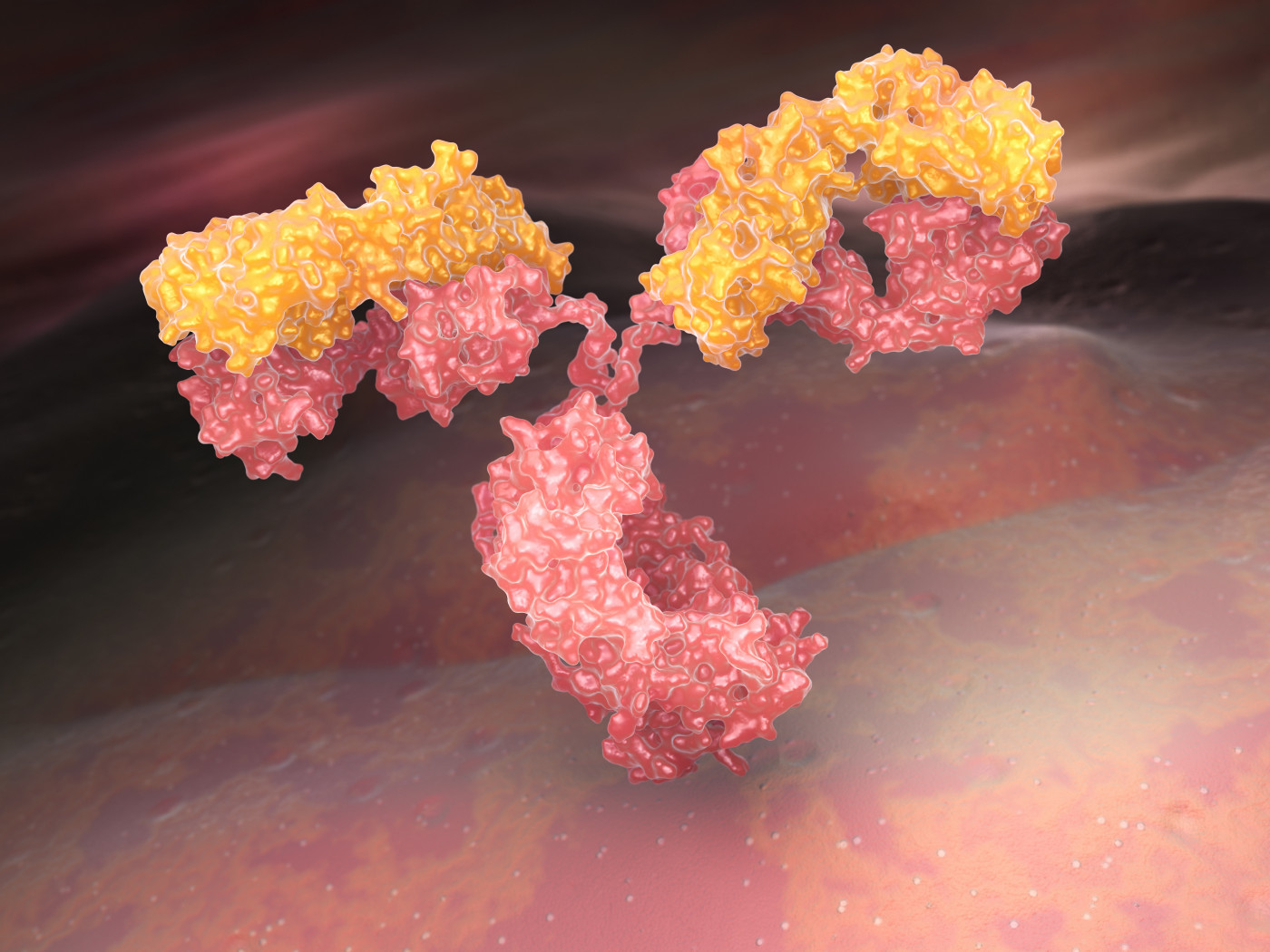
IVIG has been used for decades as a rescue medication in MG due to its rapid clinical response. The approach is prepared from a pool of immunoglobulins (antibodies) from the blood of healthy donors, which acts to neutralize and block the production of autoantibodies.
As maintenance therapies, both IVIG and SCIG have been recommended for gMG patients to spare the use of corticosteroids or as a temporary medication while these treatments take effect. In fact, regular immunoglobulin treatments are now emerging as a viable option for the long-term management of MG.
To further investigate this treatment option, researchers at the University of Toronto in Canada analyzed the medical records of 34 gMG patients who had transitioned to regular IVIG therapy and then to SCIG for long-term treatment.
Participants were between the ages of 24 and 81 (mean age 58.9) with a disease duration between three and 35 years, and were treated with immunoglobulins for at least six months during the study period (January 2015 to January 2020).
The immunosuppressive medication prednisone had been used in 30 patients (88%). All patients had received some form of immunosuppressive medication. IVIG was used by 24 patients to treat acute exacerbations, or myasthenic crisis — a severe weakening of muscles resulting in respiratory failure.
Of the 34 patients, three received SCIG infusions only, and one underwent only IVIG infusions. For the remaining 30 patients, who had IVIG followed by SCIG, the mean duration of IVIG therapy was 21.8 months, and the mean duration of SCIG treatment was 19.5 months.
Patients were treated 1 g/Kg/day of IVIG every four weeks and then switched to weekly SCIG infusions, ranging from 15 to 80 g per week.
The primary outcome was a change in Myasthenia Gravis Impairment Index (MGII) after treatment. Higher MGII scores reflect higher disability.
Results revealed a significant reduction in MGII scores from a mean of 27.7 before treatment, or baseline, to 22 after IVIG. The improvements started with IVIG treatment stabilized during the SCIG period with a mean MGII score of 19.5.
A patient-reported outcome called “percentage of normal” showed high scores associated with both treatments, increasing from 60.9% at baseline to 72.4% after IVIG treatment and 72.3% with SCIG. In turn, better scores in “percentage of normal” were linked with lower (improved) MGII scores after both treatments.
Three patients achieved minimal symptoms at the end of follow-up with no weakness and no MG-related impairments that affected daily activities. Their “percentage of normal” score was 95%.
Also, the use of immunosuppressants, prednisone and of Mestinon (pyridostigmine, manufactured by Bausch Health) lowered with chronic Ig treatment.
Having a thymoma, a tumor of the thymus — seen in 11 participants — did not significantly influence MGII score after treatment.
Only minor side effects were reported with SCIG therapy, which included headache, chills, and infusion site reaction in one patient.
In those who switched from IVIG to SCIG, 90% (27 of 30) preferred the subcutaneous (under-the-skin) route.
“Our study results suggest that patients can be successfully transitioned to IVIG and from IVIG to SCIG in the chronic treatment of gMG with reductions in impairments and use of other medications and improvement in overall status with Ig therapy,” the scientists wrote.
“Prospective, randomized studies are needed to clarify costs and comparative effectiveness,” they added.






