Patterns of Muscle Weakness in MG Patients Tend to Shift, Study Finds
People with myasthenia gravis suffer from diverse patterns of muscle weakness, which tend to shift frequently throughout the disease’s course, a new study shows.
The study, “Heterogeneity and Shifts in Distribution of Muscle Weakness in Myasthenia Gravis,” was published in the journal Neuromuscular Disorders.
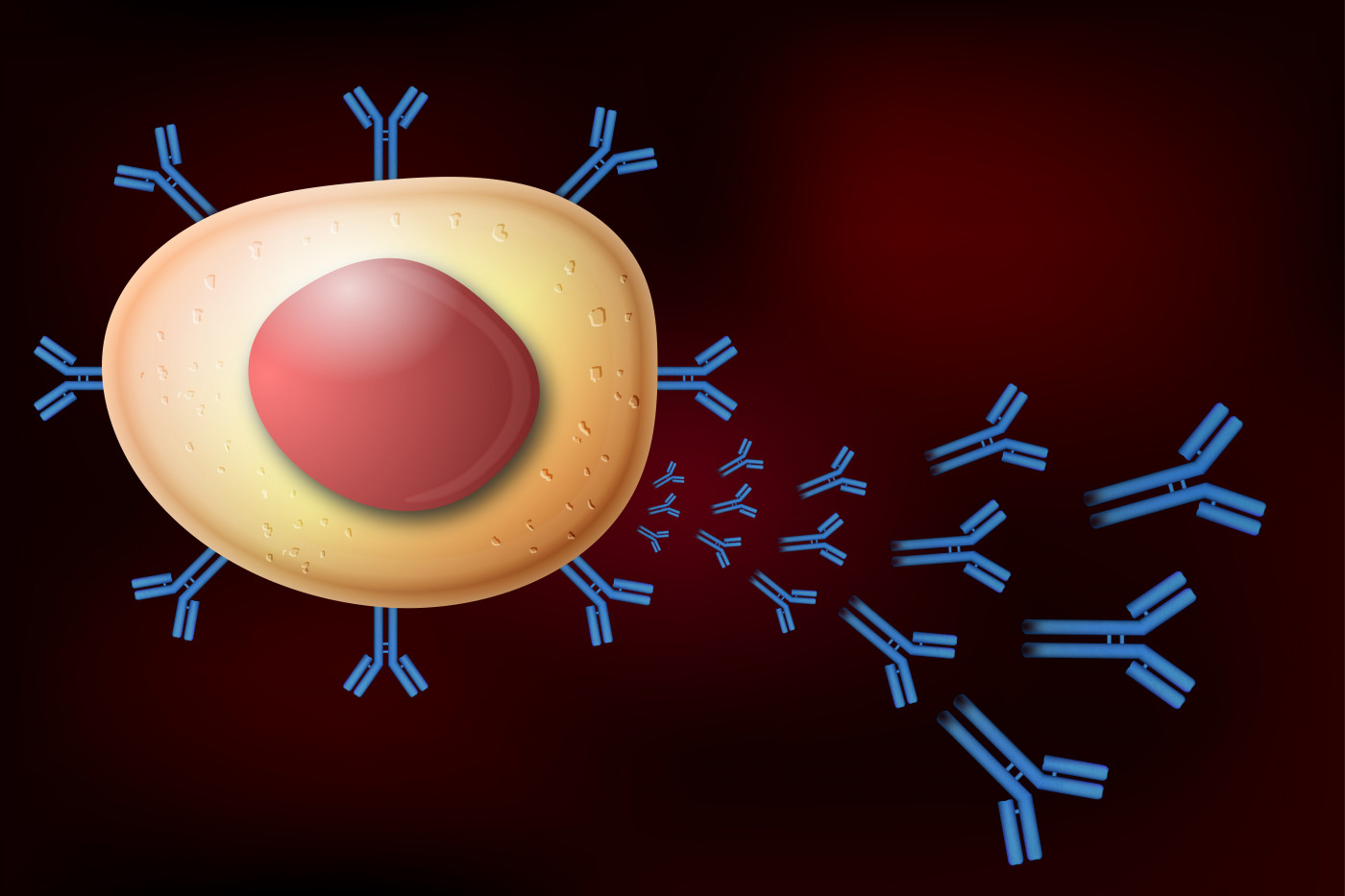
Myasthenia gravis (MG) is an autoimmune disease in which a patient’s own antibodies attack healthy proteins — known as antigens — in the body.
The most frequent antigen target is the acetylcholine receptor (AChR). Antibodies against this receptor are present in about 85 percent of MG patients.
While exposure to circulating antibodies should be similar for all types of muscles, physicians observe that there are different patterns of muscle weakness in individual patients.
To date, it is still not fully understood why there is such as a large amount of diversity (i.e. heterogeneity) that is observed in regard to patterns of muscle weakness in people with MG.
Understanding the cause of different muscle weakness patterns in MG patients might help inform treatment choices and clinical trials, as some studies show that patients with ocular (eye-related) or generalized weakness respond distinctly to different therapies.
In order to learn more about the heterogeneity of muscle weakness in MG patients, researchers systematically analyzed the distribution of muscle weakness in 225 MG patients with antibodies against AChR and the shifts in this distribution at subsequent time points.
Muscle weakness was categorized into three groups: ocular (O), bulbar (which includes speech problems, chewing weakness, swallowing weakness, or facial weakness, B) and neck/limbs/respiratory (neck weakness, respiratory weakness, hand weakness, arm weakness, or leg weakness, NLR).
There were four other groups corresponding to the combination of muscle weakness including O+B, O+NLR, B+NLR, and O+B+NLR.
At baseline, 86% of patients reported experiencing ocular weakness, 76% reported bulbar weakness and 81% reported NLR weakness.
Results indicated that ocular or bulbar weakness was resolved more frequently than NLR weakness, suggesting that NLR weakness responds less well to therapy or that oculo-bulbar muscles are better able to adapt to the chronic exposure to autoantibodies.
Furthermore, patients who did not have any form of NLR weakness reported remission more often in the first six months of their disease (defined as baseline).
Thus, these results suggest that the initial type of muscle weakness present in AChR MG patients is of prognostic value.
When looking at patient characteristics, those with either O, B, or OB weakness tended to be older at disease onset and were more frequently male compared to patients with NLR, ONLR, BNLR, or the OBNLR phenotype.
At baseline, 25 patients were purely ocular in their phenotype. Twelve of these patients (48%) remained purely ocular at subsequent time points while another 12 patients reported the appearance of NLR weakness and one patient developed an oculo-bulbar weakness.
Non-ocular phenotypes (B, NLR, BNLR) were reported by 31 patients (14%) at baseline, among whom 15 (48%) never had any ocular weakness throughout their disease course.
“MG patients have heterogeneous distributions of muscle weakness and frequently shift between phenotypes,” the authors concluded.
The researchers added that these results suggest there are other factors besides AChR antibodies that are of importance in determining muscle weakness in MG and that exploring these factors may help in developing tailored approaches for treatment of MG.
“Exploring these factors may help in developing a “personalized medicine” approach in MG by taking patient phenotypes into account in future clinical trials and in day-to-day treatment decisions,” they said.






