3 Cases of MG Possibly Caused by COVID-19 Vaccination: Report
Researchers warn of 'possible new-onset MG' after vaccine
Written by |
Researchers in Italy have reported three cases of myasthenia gravis (MG) they say may possibly have been caused by a vaccine against SARS-CoV-2, the virus that causes COVID-19.
“Clinicians should be aware of possible new-onset MG after SARS-CoV-2 vaccination, especially with the current recommendation of booster doses,” the team wrote in a new report describing the trio of cases.
It is still unclear at this point if COVID-19 vaccinations are truly capable of triggering MG, the scientists stressed. But they noted that “it is conceivable that the vaccine might have triggered an immune-mediated process in predisposed subjects or most likely exacerbated [worsened] a subclinical pre-existing form of MG.”
The report, “New-onset myasthenia gravis after mRNA SARS-CoV-2 vaccination: a case series,” was published in the journal Neurological Sciences.
MG is a rare autoimmune disorder driven by self-reactive antibodies that attack molecules involved in nerve-muscle communication. It results in fatigue and muscle weakness.
Link between COVID-19 vaccine and myasthenia gravis
The disease has been associated with COVID-19 in a few case reports in the last few years. Meanwhile, COVID-19 vaccination has also been cited as a cause of myasthenic crises — episodes of MG worsening — in previously diagnosed patients. Yet, reports describing the onset of MG following COVID-19 vaccination are rare.
Now, the team in Italy described the cases of three patients, all men, who developed MG after being vaccinated against COVID-19.
Two of them, ages 90 and 80, developed MG symptoms within six to 10 days after receiving the second shot of the BioNTech/Pfizer and Moderna COVID-19 vaccines. The third patient, age 55, developed symptoms after the first shot. Those symptoms significantly worsened four weeks after receiving the second dose of the Moderna COVID-19 vaccine.
The first patient, the oldest of the three, had chronic heart and kidney disease and developed weakness, head drop, and droopiness in both eyelids. A heart ultrasound and other exams were unremarkable, giving clinicians few clues.
His symptoms continued to worsen, so he was referred to the neurology department. Further tests confirmed loss of strength in his neck muscles, causing fatigability. He had received the first dose of the BioNTech/Pfizer COVID-19 vaccine three weeks earlier, but experienced no significant side effects.
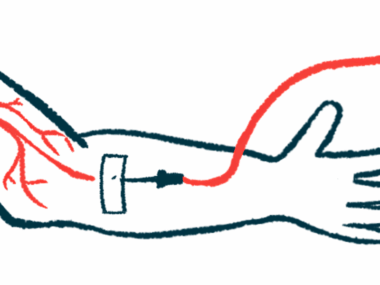
The man underwent repetitive nerve stimulation (RNS) in the facial nerve, the results of which were consistent with an MG diagnosis.
During this test, electrodes are placed on the skin over the muscle clinicians wish to test. These electrodes then send out small electrical pulses that allow doctors to measure the nerve’s ability to send these signals to muscle tissue. If signal transmission worsens with fatigue, which tends to occur after several rounds of stimulation, the patient is diagnosed with MG.
He also tested positive for antibodies against the acetylcholine receptor (AChR), the most common type of MG-causing antibodies.
The second patient, who had high blood pressure, diabetes, and high cholesterol, was treated by the neurology department for symptoms of eyelid droopiness, double vision, difficulty swallowing, and head drop. Loss of strength was seen across several muscles in the head and neck, while leg muscles were unaffected. His symptoms started six days after he was given the second shot of the Moderna vaccine.
RNS results were in agreement with MG, and he tested positive for AChR antibodies. A chest CT scan showed no abnormalities in the thymus, a gland-like organ located in the chest that is part of the immune system.
Treating new-onset MG
Both patients received treatment with pyridostigmine (sold as Mestinon, among other brand names), a medicine commonly prescribed to improve muscle strength in MG patients.
In the first patient, a dosing regimen of 30 mg of pyridostigmine three times daily was enough to control his symptoms. Due to his advanced age, no additional treatments were given. One month after discharge, there were no changes in his condition.
In the second patient, however, his condition continued to worsen despite treatment. He had five sessions of plasma exchange therapy, called plasmapheresis, which involves replacing a person’s plasma — the non-cellular part of blood. He started to improve after completing the second session.
Due to his diabetes and high cholesterol, instead of being treated with steroids, this patient received treatment with the immunosuppressant azathioprine. At his hospital discharge, his neurological exams were normal, with the exception of a slight droopiness in his right eyelid. This was still visible at his three-month follow-up, but there were no signs of low muscle strength. The levels of AChR antibodies in the blood had also dropped.
The third patient, the youngest of the men, had symptoms of weakness in the upper limb muscles, as well as in the neck, and had double vision. He complained of pain in the neck and difficulty breathing when lying down, a condition called orthopnea.
This man’s neurological examination confirmed he had double vision, muscle weakness, and fatigability in neck muscles and in the upper body. Weakness and fatigability also affected the muscles in his legs, but to a lesser extent.
His symptoms began three days after he received the first dose of the Moderna COVID-19 vaccine, and became significantly worse after the second dose, which was given four weeks later.
As with the other patients, findings in the RNS test of his left facial muscles and levels of AChR antibodies in the blood were consistent with an MG diagnosis.
His condition improved after treatment with pyridostigmine and a five-day course of intravenous immunoglobulin (IVIG).
Upon his discharge from the hospital, he still showed eyelid droopiness in his left eye, but no other symptoms. He was prescribed a daily dose of pyridostigmine and prednisone.
During his follow-up three months later, the patient still showed a mild upper limb weakness, but no signs of bulbar symptoms — those involving the face and neck — or eye involvement were detected.
“This case series highlights the importance of recognizing rare immune-mediated disorders temporally related to SARS-CoV-2 vaccination. Whether the vaccine is causally related to the development of MG or a random occurrence is not clear and supporting evidences on a causal relationship are scarce,” the researchers wrote.
“The hyperstimulation of the innate immune system or the exacerbation of a subclinical pre-existing MG could be possible explanations,” they wrote.


Leave a comment
Fill in the required fields to post. Your email address will not be published.