Low-dose course of rituximab effective for MuSK-MG: Small study
Researchers reviewed data from 8 women, 1 man assigned to the regimen
Written by |
A treatment course of low-dose rituximab eased measures of clinical severity, improved quality of life, and allowed lower steroid doses to be used in myasthenia gravis (MG) patients who have antibodies against muscle-specific tyrosine kinase (MuSK).
That’s according to a small study in China that looked at a median of one year of follow-up data from 10 patients receiving this regimen.
“To fully ascertain the long-term effectiveness and safety of this therapy, additional research is required,” the researchers wrote in “Promising efficacy of Low-Dose rituximab in Muscle specific kinase antibody positive Myasthenia Gravis,” which was published in Neuroscience Letters.
In MG, self-reactive antibodies attack key proteins that mediate nerve-muscle communication, causing muscle weakness. While these antibodies mostly target the acetylcholine receptor protein (AChR), around 4-5% of patients have antibodies against the MuSK protein.
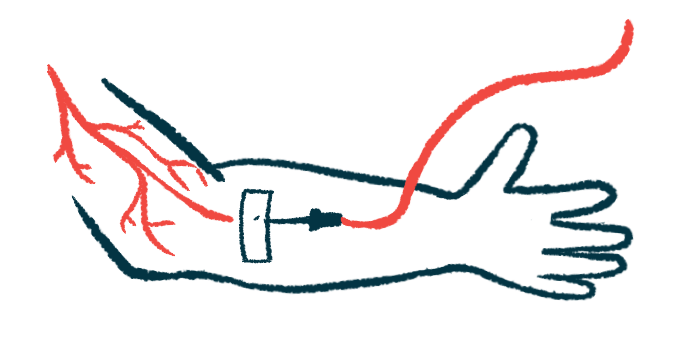
Rituximab, sold under the brand name Rituxan and others, with biosimilars available, is an antibody-based therapy that targets and destroys B-cells, the immune cells that produce the damaging antibodies in MG.
While it isn’t approved for MG, rituximab is often used off-label for patients who fail to respond to standard treatments, and beneficial effects have been reported. Also, “several case reports and clinical series have shown [rituximab] is effective for treating Musk-MG even better than AChR-MG,” the researchers wrote.
Low-dose rituximab
In most MG studies, rituximab was administered in either four weekly doses of 375 mg/m2 or at 1,000 mg on day 1 and day 15, with redosing every six months.
However, “the most effective dosages of [rituximab] infusions remain unsolved,” wrote researchers at the First Affiliated Hospital of Shanxi Medical University, China who implemented a low-dose rituximab regimen as the standard treatment for MuSK-MG patients at their hospital to reduce costs and minimize possible side effects associated with a high dose.
The course consisted of a three-day induction period of 500 mg — 100 mg on the first day followed by 200 mg on the second and third day, then 500-mg infusions every six months or every year.
The researchers described the therapeutic efficacy of this approach following a review of data from eight women and one man with MuSK-MG who were treated with this regimen anytime between April 2021 to April 2023. The patients’ disease duration ranged between three months and about 4.5 years. Seven patients (77.8%) had previously been given immunosuppressive treatments, including tacrolimus and the corticosteroid prednisolone.
During these treatments, eight patients (88.9%) also received the first-line MG therapy pyridostigmine bromide, which is sold as Mestinon and has generics available. Three patients had a myasthenic crisis, a sudden worsening of MG symptoms, and four others were in a pre-crisis state. Myasthenic crises were treated with either intravenous immunoglobulin, which is intended to neutralize self-reactive antibodies, or a high-dose steroid pulse plus rituximab.
After that, the nine MuSK-MG patients received one to four cycles of the low-dose rituximab regimen, with a median follow-up of 13 months (range, three months to nearly two years).
The treatment’s effectiveness was assessed through changes in the MG Foundation of America (MGFA) scale and the MGFA-Post Intervention Status (MGFA-PIS), as well as in the dose of steroids needed, since long-term use and high doses of these medications are associated with serious side effects.
Before the low-dose regimen, two patients had mild weakness, four had moderate weakness, and three needed to be intubated to help them breathe, according to their MGFA scores.
At the final follow-up after treatment, all nine showed clinical improvements based on their MGFA scores. Four (44.4%) no longer showed symptoms and the remaining five (55.6%) were categorized with mild weakness that mainly affected the limbs or the respiratory muscles.
Improvements in MGFA-PIS were also reported, with four (44.4%) patients achieving pharmacologic remission and two (22.2%) showing minimal manifestations. Three (33.3%) saw functional improvement, but still had symptoms.
The mean dose of prednisolone was significantly reduced after the low-dose rituximab regimen, from 50 mg at the start of treatment to 18.3 mg at the last follow-up. Two patients reduced their daily prednisolone dose to 10 mg or less.
By the end of the follow-up, significant improvements were seen in the ability to perform daily activities and quality of life. Median Quantitative Myasthenia Gravis scores were also significantly reduced, indicating less severe disease.
The observed benefits of the low-dose rituximab regimen were seen “regardless of whether patients had previously received immunosuppressive treatments,” said the researchers.
The rituximab course was generally well tolerated with no serious side effects reported.
“Our study provides evidence supporting the potential of low-dose [rituximab] as a promising, effective treatment for patients with Musk- MG,” wrote the researchers, who said larger studies that follow patients over time should confirm these findings. A larger, controlled trial could clarify the benefits of low-dose rituximab in MuSK-MG patients, they said.







Leave a comment
Fill in the required fields to post. Your email address will not be published.