Patients with FSHD Can Develop Myasthenia Gravis, Report Indicates
Patients with facioscapulohumeral dystrophy (FSHD) — a type of muscular dystrophy — can develop myasthenia gravis, possibly because of underlying immune dysfunction.
A letter to the editor describing the case, titled “A case of facioscapulohumeral muscular dystrophy and myasthenia gravis with positivity of anti-Ach receptor antibody: a fortuitous association?” was published in the journal Neurological Sciences.
FSHD, the third-most common form of muscular dystrophy, presents with slowly progressing weakness that affects the face, shoulder, and arms.
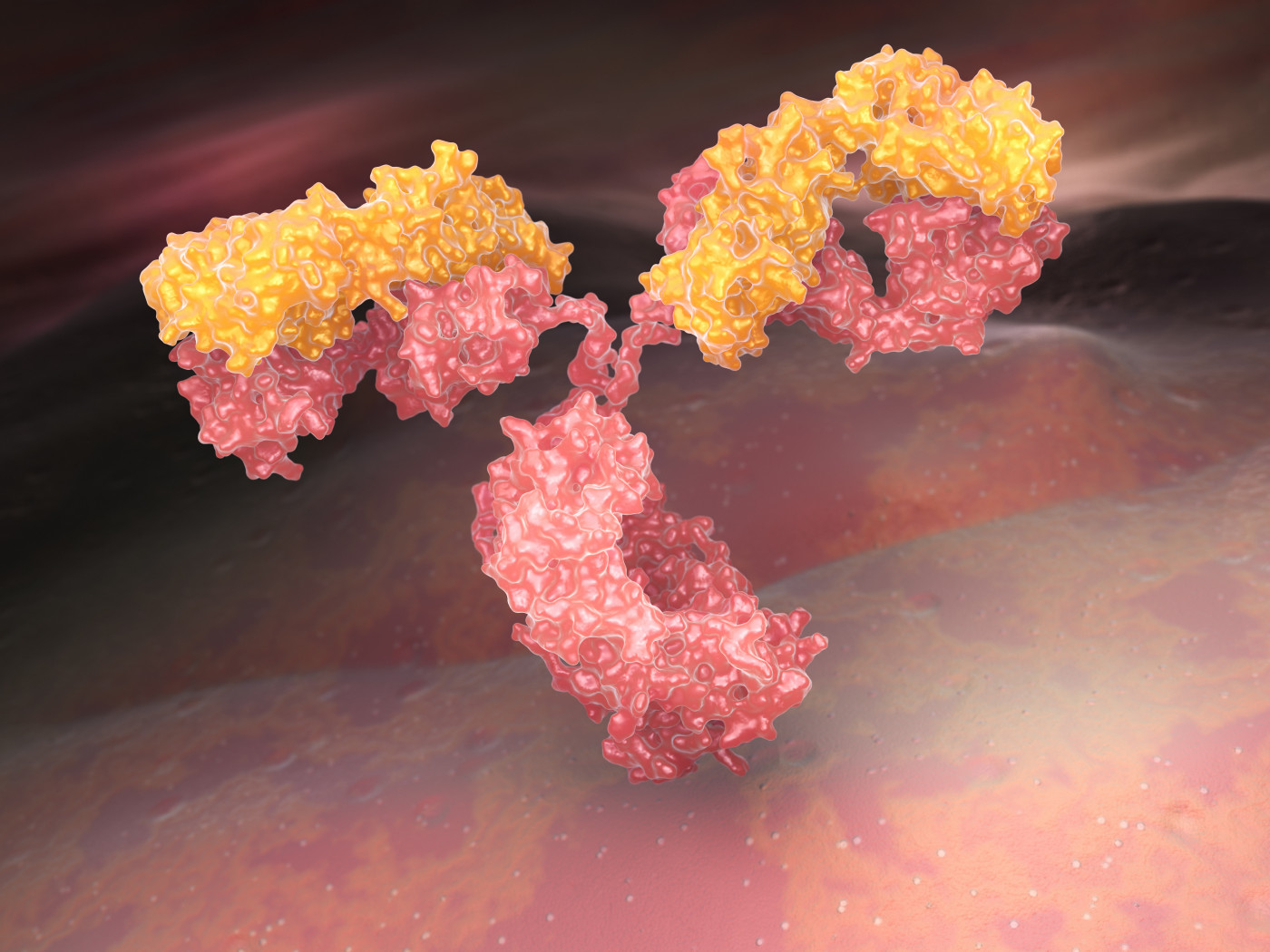
Myasthenia gravis (MG) is an autoimmune disease characterized by the presence of antibodies that attack the the anti-acetylcholine receptor, which is involved in signaling between nerve and muscle cells at a location called the neuromuscular junction.
According to reports in literature, the simultaneous occurrence of FSHD and MG is infrequent. However, in this case report, physicians present the case of a patient who had a history of FSHD and then developed MG.
A 69-year-old woman, diagnosed with FSHD 13 years previously, came to a clinic complaining of dysphagia (difficulty swallowing), weakness of all limbs, and double vision.
To investigate the cause of muscle weakness, physicians conducted a neurophysiological test known as concentric needle electromyography (EMG), used to assess the health of muscles and the nerve cells that control them.
EMG findings suggested that the patient had myopathy — a condition in which muscle fibers do not work properly.
Physicians also conducted repetitive nerve stimulation (RNS), a test used to diagnose neuromuscular junction (NMJ) disorders. Results suggested a diagnosis of MG. This was confirmed by the detection of autoantibodies against the anti-acetylcholine receptor.
The patient was administered intravenous immunoglobulin therapy for five days and then started on mestinon (pyridostigmine), which resulted in significant improvement on both clinical and electrophysiological parameters.
At follow-up a year later, the patient continued to show substantial stability, both clinically and electrophysiologically.
As FSHD and MG are rare diseases, the occurrence of both in one person seems unlikely to be coincidental.
The authors speculated that the occurrence of MG and FSHD suggests that there are immune mechanisms at play in patients with FSHD.
The muscular degeneration that occurs in FSHD may act as a trigger for the immune system to produce high levels of anti-acetylcholine receptor antibodies — leading to the development of MG —particularly in patients already predisposed to autoimmune diseases such as arthritis.
The authors conclude that “there are limited reports of concomitant occurrence of FSHD and MG in the literature, but this association must be considered, to avoid a dangerous diagnostic delay, when any unusual changes in the course of disease or development of unusual symptoms appear, as this case shows.”






